Type 2 diabetes mellitus (T2DM) is a chronic metabolic disorder characterized by insulin resistance and progressive beta-cell dysfunction, resulting in hyperglycemia. It accounts for over 90% of all diabetes cases globally and has become a major public health concern due to its rapidly rising prevalence and strong association with obesity, sedentary lifestyles, and aging populations.

Understanding the Pathophysiology of Type 2 Diabetes Mellitus
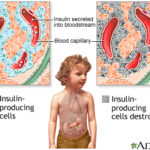
Type 2 diabetes is primarily driven by two key mechanisms:
- Insulin resistance: Reduced sensitivity of peripheral tissues—particularly muscle, fat, and liver—to insulin action.
- Beta-cell dysfunction: Gradual impairment in insulin secretion from pancreatic beta-cells.
These factors interact to create a state of chronic hyperglycemia, eventually leading to the clinical manifestation of T2DM.
Causes and Risk Factors of Type 2 Diabetes Mellitus
Several modifiable and non-modifiable risk factors contribute to the development of type 2 diabetes:
Non-Modifiable Factors
- Genetics: Family history significantly increases risk.
- Age: Incidence rises after age 45.
- Ethnicity: Higher prevalence among African Americans, Hispanics, Native Americans, and South Asians.
Modifiable Factors
- Obesity, particularly visceral fat
- Physical inactivity
- Poor dietary habits
- Hypertension and dyslipidemia
- Gestational diabetes history
Clinical Presentation: Recognizing the Symptoms of T2DM
Symptoms of type 2 diabetes may be subtle or absent in early stages. Common clinical signs include:
- Polyuria (frequent urination)
- Polydipsia (excessive thirst)
- Polyphagia (increased hunger)
- Unexplained weight loss
- Fatigue and irritability
- Blurred vision
- Slow-healing wounds
- Frequent infections
Many individuals remain asymptomatic and are diagnosed during routine screenings or when complications arise.
Diagnostic Criteria for Type 2 Diabetes Mellitus
Diagnosis of T2DM is based on specific glycemic thresholds established by the American Diabetes Association (ADA):
| Test | Diagnostic Threshold |
|---|---|
| Fasting Plasma Glucose (FPG) | ≥ 126 mg/dL (7.0 mmol/L) |
| 2-h Plasma Glucose (OGTT) | ≥ 200 mg/dL (11.1 mmol/L) |
| Hemoglobin A1c (HbA1c) | ≥ 6.5% |
| Random Plasma Glucose | ≥ 200 mg/dL with symptoms |
A confirmatory test on a different day is typically recommended unless hyperglycemia with symptoms is evident.
Complications of Type 2 Diabetes Mellitus
T2DM can lead to severe microvascular and macrovascular complications if not adequately managed.
Microvascular Complications
- Diabetic retinopathy: Leading cause of adult blindness
- Diabetic nephropathy: Progressive kidney damage
- Diabetic neuropathy: Peripheral and autonomic nerve damage
Macrovascular Complications
- Cardiovascular disease: Increased risk of heart attacks and strokes
- Peripheral artery disease: Can lead to foot ulcers and amputations
Early detection and aggressive glycemic control significantly reduce the risk of these complications.
Type 2 Diabetes Management Strategies
Effective T2DM management requires a multifaceted approach involving lifestyle interventions, pharmacotherapy, and regular monitoring.
Lifestyle Modifications
Diet
- Emphasize complex carbohydrates, fiber, and lean protein
- Minimize refined sugars and saturated fats
- Portion control and caloric reduction for weight loss
Physical Activity
- Minimum 150 minutes per week of moderate aerobic activity
- Include resistance training to improve insulin sensitivity
Weight Management
- Target 5–10% reduction in body weight
- Bariatric surgery may be considered for individuals with BMI ≥35 kg/m²
Pharmacological Treatments
First-Line Therapy
- Metformin: Improves insulin sensitivity and reduces hepatic glucose production
Second-Line Options
- SGLT2 inhibitors (e.g., empagliflozin): Promote urinary glucose excretion
- GLP-1 receptor agonists (e.g., liraglutide): Improve glycemic control and promote weight loss
- DPP-4 inhibitors (e.g., sitagliptin): Prolong incretin hormone activity
- Thiazolidinediones (e.g., pioglitazone): Enhance peripheral insulin sensitivity
- Sulfonylureas (e.g., glimepiride): Stimulate insulin secretion
Insulin Therapy
- Required when oral agents fail or in cases of marked hyperglycemia
- Basal-bolus regimens or premixed insulin formulations may be used
Monitoring and Glycemic Targets
Ongoing monitoring is essential to prevent complications and assess treatment effectiveness.
| Parameter | Recommended Goal |
|---|---|
| HbA1c | <7.0% (individualized) |
| Fasting glucose | 80–130 mg/dL |
| Postprandial glucose | <180 mg/dL |
| Blood pressure | <140/90 mmHg |
| LDL cholesterol | <100 mg/dL (or <70 mg/dL if CVD present) |
Continuous glucose monitoring (CGM) may benefit selected patients, particularly those on insulin.
Prevention and Early Intervention
For individuals with prediabetes, early intervention can delay or prevent the progression to T2DM.
Evidence-Based Prevention Measures
- Intensive lifestyle modification programs
- Weight loss of 7–10%
- 150+ minutes/week of moderate physical activity
- Consider metformin in high-risk individuals (e.g., BMI ≥35, age <60, history of gestational diabetes)
Special Populations and Considerations
Elderly Patients
- Individualized glycemic goals to balance risk of hypoglycemia
- Prioritize quality of life and function
Pregnant Women
- T2DM may require insulin during pregnancy
- Intensive monitoring is critical for maternal and fetal outcomes
Adolescents and Young Adults
- Increasing prevalence due to rising childhood obesity
- Require aggressive management and psychological support
Future Directions in Type 2 Diabetes Care
Advancements in diabetes care continue to reshape treatment paradigms:
- Precision medicine: Tailoring therapy based on genetic, phenotypic, and metabolic profiles
- Smart insulin delivery: Integration of insulin pumps with CGM
- Dual and triple agonists: Combining GLP-1, GIP, and glucagon receptor activity
- Artificial pancreas: Closed-loop insulin delivery systems
Type 2 diabetes mellitus is a multifactorial chronic disease with far-reaching health consequences. Effective management hinges on early diagnosis, sustained lifestyle changes, personalized pharmacologic therapy, and vigilant monitoring. As scientific understanding and therapeutic options evolve, a patient-centric, integrated care model remains essential to reducing the global burden of T2DM.