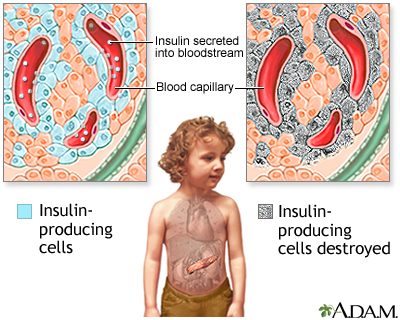
Type 1 diabetes mellitus (T1DM) is a chronic autoimmune disorder that results in the destruction of pancreatic beta cells, leading to absolute insulin deficiency. Unlike type 2 diabetes, T1DM typically presents early in life, although adult onset is also possible. Early diagnosis and precise management are crucial to preventing acute complications and long-term organ damage.
Understanding Type 1 Diabetes Mellitus
T1DM occurs when the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This autoimmune destruction causes elevated blood glucose levels due to the body’s inability to produce insulin.
Key Characteristics of T1DM
- Absolute insulin deficiency
- Autoimmune etiology
- Usually diagnosed in children, adolescents, or young adults
- Requires lifelong insulin therapy
Causes and Risk Factors of Type 1 Diabetes
While the exact cause of T1DM remains uncertain, a combination of genetic predisposition and environmental triggers is believed to initiate the autoimmune process.
Genetic Susceptibility
- HLA-DR3/DR4-DQ8 genes: Strongly associated with T1DM development
- Family history: A first-degree relative with T1DM increases the risk significantly
Environmental Triggers
- Viral infections: Enteroviruses (e.g., coxsackievirus) may act as triggers
- Early childhood diet: Exposure to cow’s milk or gluten at an early age has been studied
- Vitamin D deficiency: May play a role in immune dysregulation
Signs and Symptoms of Type 1 Diabetes Mellitus
T1DM symptoms often present suddenly and can be severe if not recognized early. The classic triad of symptoms includes:
- Polyuria: Frequent urination due to osmotic diuresis
- Polydipsia: Increased thirst from dehydration
- Polyphagia: Increased hunger as cells are starved of glucose
Additional Symptoms
- Weight loss despite normal or increased appetite
- Fatigue and weakness
- Blurred vision
- Irritability or mood changes
- Diabetic ketoacidosis (DKA) in severe cases
Diagnostic Criteria for Type 1 Diabetes
Diagnosis is based on blood glucose testing and clinical presentation.
Laboratory Tests
- Fasting Plasma Glucose (FPG) ≥ 126 mg/dL
- Random Plasma Glucose ≥ 200 mg/dL with symptoms
- Oral Glucose Tolerance Test (OGTT) ≥ 200 mg/dL after 2 hours
- Hemoglobin A1c (HbA1c) ≥ 6.5%
- C-peptide Test: Low levels indicate reduced insulin production
- Autoantibody Testing: Positive for GAD65, IA-2, or ZnT8 antibodies
Treatment and Management of Type 1 Diabetes
Effective management of T1DM requires a comprehensive, multidisciplinary approach focused on insulin therapy, blood glucose monitoring, lifestyle modifications, and patient education.
Insulin Therapy
Insulin is the cornerstone of T1DM treatment. Various insulin regimens are available:
- Basal-Bolus Regimen: Combines long-acting (basal) and rapid-acting (bolus) insulins
- Insulin Pumps: Provide continuous subcutaneous insulin infusion
- Closed-Loop Systems: Artificial pancreas integrating CGM and insulin pump
Blood Glucose Monitoring
- Self-Monitoring of Blood Glucose (SMBG): Frequent testing using glucometers
- Continuous Glucose Monitoring (CGM): Real-time glucose data for trend analysis
Nutritional and Lifestyle Considerations
Dietary Management
- Carbohydrate Counting: Helps adjust insulin doses based on meal content
- Glycemic Index Awareness: Focus on low-GI foods to minimize spikes
- Balanced Macronutrients: Adequate intake of proteins, fats, and fiber
Physical Activity
- Regular aerobic and resistance exercises improve insulin sensitivity
- Monitor for hypoglycemia during and after exercise sessions
Acute and Chronic Complications of T1DM
Acute Complications
- Diabetic Ketoacidosis (DKA): Life-threatening condition with high blood glucose, ketones, and acidosis
- Hypoglycemia: Caused by excess insulin, delayed meals, or vigorous exercise
Chronic Complications
| System Affected | Complications |
|---|---|
| Cardiovascular | Hypertension, coronary artery disease |
| Renal | Diabetic nephropathy |
| Ocular | Diabetic retinopathy, cataracts |
| Neurological | Peripheral neuropathy, autonomic neuropathy |
| Dermatological | Diabetic dermopathy |
Regular screening and early intervention are critical in preventing or delaying complications.
Psychosocial Impact and Support Systems
Living with T1DM can significantly affect mental and emotional well-being. Structured support is essential:
- Psychological counseling: Managing anxiety, burnout, and depression
- Diabetes education programs: Empowering patients with self-care skills
- Family and peer support: Vital for children and adolescents with diabetes
Advances in Type 1 Diabetes Research and Technology
Ongoing innovation is reshaping the T1DM management landscape:
Technological Developments
- Artificial pancreas systems with automated insulin delivery
- Smart insulin pens with dose tracking
- Mobile health apps for real-time monitoring and support
Research Frontiers
- Beta cell replacement therapies (islet transplantation, stem cells)
- Immunomodulatory treatments to prevent or halt autoimmune attack
- Genetic screening for early identification and prevention
Type 1 diabetes mellitus is a complex, lifelong condition that requires personalized and proactive care. With advancements in insulin delivery, glucose monitoring, and medical technology, individuals with T1DM can lead healthy, productive lives. Early diagnosis, consistent monitoring, and collaborative management remain the pillars of optimal outcomes.
FAQs
What causes type 1 diabetes mellitus?
T1DM is caused by an autoimmune attack on pancreatic beta cells, influenced by genetic and environmental factors.
Can type 1 diabetes be cured?
Currently, there is no cure. However, research into beta cell regeneration and immune therapies is ongoing.
How is type 1 diabetes managed?
Management includes insulin therapy, blood glucose monitoring, dietary planning, exercise, and education.
Is type 1 diabetes hereditary?
Genetics play a role, but not all individuals with a family history develop the condition. Environmental triggers also contribute.
What are the early symptoms of type 1 diabetes?
Increased thirst, frequent urination, unexplained weight loss, and fatigue are common early signs.