Tuberculosis (TB) prophylaxis represents a critical component of global TB control strategies. It involves targeted interventions to prevent latent TB infection (LTBI) from progressing to active disease or to protect uninfected individuals from acquiring Mycobacterium tuberculosis (M. tuberculosis). This is particularly vital among high-risk groups such as immunocompromised individuals, close contacts of infectious TB cases, and healthcare workers.
Understanding the Basis of TB Prophylaxis
TB is transmitted via airborne droplets from individuals with pulmonary or laryngeal TB. Once inhaled, M. tuberculosis can establish a latent infection that may later progress to active disease. The primary goal of prophylaxis is to:
- Eliminate latent bacilli before activation
- Reduce TB incidence and transmission
- Protect vulnerable populations
Indications for TB Prophylaxis
1. Close Contacts of Active TB Cases
- Household or frequent contact with pulmonary TB patients
- Children under 5 years old in contact with smear-positive cases
2. HIV-Infected Individuals
- Significantly increased risk of reactivation
- Prophylaxis recommended even if latent TB test is negative
3. Patients on Immunosuppressants
- Those receiving TNF-alpha inhibitors, corticosteroids, or post-transplant therapy
4. Individuals with Positive Tuberculin Skin Test (TST) or IGRA
- Without evidence of active disease on radiography or symptoms
Tuberculosis Prophylaxis Regimens
Isoniazid Preventive Therapy (IPT)
Standard Regimen:
- Drug: Isoniazid (INH)
- Duration: 6 to 9 months
- Dosage: 5 mg/kg daily (maximum 300 mg/day)
- Pyridoxine (Vitamin B6): Co-administered to prevent neuropathy
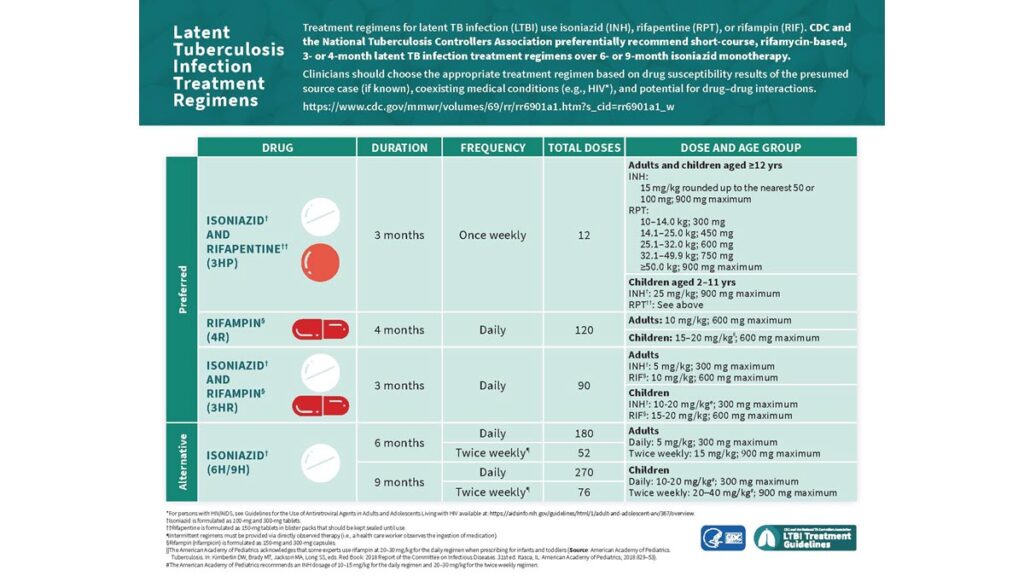
Rifamycin-Based Regimens
These are shorter and equally effective alternatives to IPT.
3HP Regimen (12-Dose Weekly Therapy)
- Drugs: Isoniazid + Rifapentine
- Duration: 12 weeks (once-weekly)
- Advantages: High completion rates and safety
- Indications: Adults and children >2 years, including HIV-infected (non-pregnant)
1HP Regimen
- Drugs: Isoniazid + Rifapentine
- Duration: Daily for 1 month
- Target Group: HIV-infected adults
4R Regimen
- Drug: Rifampicin
- Duration: 4 months
- Use Case: INH intolerance or resistance
Special Considerations for TB Prophylaxis
HIV and TB Co-infection
- TB remains a leading cause of death among people with HIV.
- IPT or rifamycin-based therapy significantly reduces TB risk.
- ART and TB prophylaxis should be integrated.
Pediatric Populations
- Children under 5 in contact with TB cases must receive prophylaxis.
- INH for 6 months remains standard.
- Ensure active TB is ruled out before initiating therapy.
Pregnant and Lactating Women
- INH is considered safe during pregnancy.
- Pyridoxine supplementation is essential.
- Rifapentine-based regimens are avoided due to limited safety data.
Monitoring and Management During Prophylaxis
Baseline Evaluations:
- Clinical assessment
- Chest radiograph
- Liver function tests (in high-risk groups)
During Treatment:
- Monthly follow-ups for adherence and adverse effect monitoring
- Discontinuation if active TB develops
Common Side Effects:
- Hepatotoxicity
- Peripheral neuropathy (INH)
- Rash, GI upset (rifamycins)
TB Prophylaxis in Healthcare and Institutional Settings
Healthcare Workers
- Regular screening with TST or IGRA
- Prophylaxis if LTBI is detected
- Environmental controls to reduce exposure
Correctional Facilities and Shelters
- Congregate settings are high-risk for transmission
- Routine screening and mass prophylaxis may be considered
Global Guidelines and National Programs
WHO Guidelines
- Recommend TB preventive treatment (TPT) for all HIV-positive individuals, children under 5 in contact with TB, and household contacts of MDR-TB cases (after ruling out active TB)
- End TB Strategy includes scaling up TPT coverage
National Tuberculosis Elimination Program (NTEP) – India
- INH prophylaxis for under-5 children and PLHIV
- Expanding use of shorter regimens such as 3HP
- TB preventive services integrated into routine HIV care
Future Directions in TB Prophylaxis
Biomarker-Guided Prophylaxis
- Predicting individuals at highest risk of reactivation
- Customizing treatment duration and intensity
New Drug Regimens
- Investigations into fluoroquinolone-based and newer rifamycin formulations
- Potential use of long-acting injectable prophylaxis
Vaccination Approaches
- BCG efficacy wanes with age and does not prevent reactivation
- Trials underway for vaccines targeting LTBI and adult TB prevention
Prioritizing Prevention for TB Elimination
Tuberculosis prophylaxis remains a cornerstone in the global fight against TB. The strategic implementation of preventive therapy in high-risk groups not only reduces individual disease risk but also interrupts community-level transmission. Widespread awareness, accurate diagnosis of latent infection, and adherence to short, effective treatment regimens are imperative to achieving the global goal of TB elimination.