Tuberculosis meningitis (TBM), also known as tuberculous meningitis, is the most severe form of extrapulmonary tuberculosis, involving inflammation of the meninges due to Mycobacterium tuberculosis. TBM presents significant diagnostic and therapeutic challenges and is associated with high morbidity and mortality, especially in resource-limited settings.
Pathogenesis of TB Meningitis
Tuberculosis meningitis develops as a complication of primary or reactivated pulmonary TB. The infection disseminates hematogenously to the central nervous system (CNS), forming Rich foci—small granulomatous lesions—that eventually rupture into the subarachnoid space, initiating a meningeal inflammatory response.
Epidemiology and Risk Factors
Tuberculosis meningitis predominantly affects:
- Children under 5 years
- Immunocompromised individuals (especially those with HIV)
- Individuals in TB-endemic regions
Key Risk Factors:
- Active or previous pulmonary TB
- HIV infection
- Malnutrition
- Diabetes mellitus
- Poor access to healthcare
Clinical Presentation of Tuberculosis Meningitis
The symptoms of TB meningitis often develop insidiously over several days to weeks and progress through three clinical stages.
Stage I: Prodromal Phase
- Low-grade fever
- Malaise
- Headache
- Irritability
Stage II: Meningeal Phase
- Neck stiffness
- Photophobia
- Vomiting
- Lethargy
- Cranial nerve palsies (especially VI and VII)
Stage III: Paralytic Phase
- Seizures
- Hemiparesis or paraplegia
- Coma
- Death if untreated
Diagnostic Evaluation of TB Meningitis
Timely diagnosis is crucial but often delayed due to non-specific early symptoms.
Lumbar Puncture and CSF Analysis:
- High opening pressure
- Elevated protein (>100 mg/dL)
- Low glucose (<40 mg/dL)
- Lymphocytic pleocytosis
Confirmatory Tests:
- CSF AFB stain (low sensitivity)
- CSF culture for M. tuberculosis (gold standard, but slow)
- Nucleic acid amplification tests (e.g., Xpert MTB/RIF Ultra)
- CSF adenosine deaminase (ADA) may support diagnosis
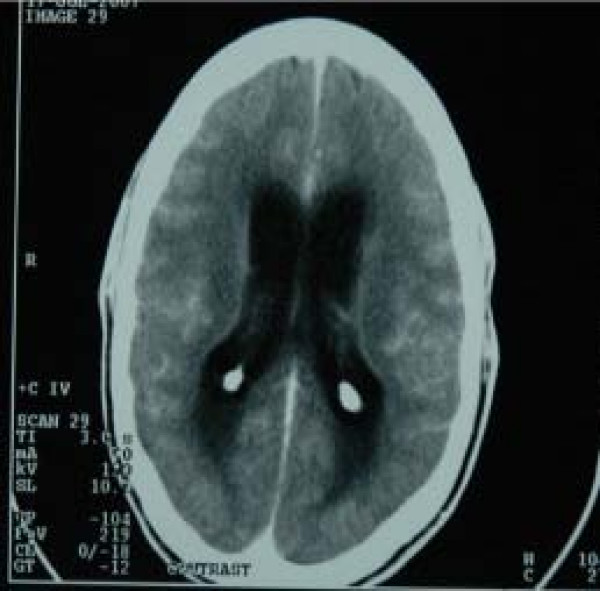
Imaging:
- MRI with contrast is preferred; findings may include:
- Basal meningeal enhancement
- Hydrocephalus
- Infarcts
- Tuberculomas
Differential Diagnosis
TB meningitis must be differentiated from other causes of chronic meningitis:
- Viral meningitis (especially HSV and enteroviruses)
- Cryptococcal meningitis (particularly in HIV patients)
- Carcinomatous meningitis
- Neurosarcoidosis
- Fungal meningitis (e.g., Candida, Histoplasma)
Treatment of Tuberculous Meningitis
Antitubercular Therapy (ATT):
A prolonged course of ATT is essential.
Initial Phase (2 months):
- Isoniazid
- Rifampicin
- Pyrazinamide
- Ethambutol
Continuation Phase (10 months or longer):
- Isoniazid
- Rifampicin
Adjunctive Corticosteroids:
- Dexamethasone or Prednisolone reduces mortality and neurological complications.
- Particularly beneficial in patients with raised intracranial pressure or cerebral edema.
Management of Complications:
- Hydrocephalus: May require ventriculoperitoneal shunt or external ventricular drainage.
- Seizures: Antiepileptic therapy.
- Hyponatremia: Often due to SIADH or cerebral salt wasting; managed accordingly.
Prognosis and Long-Term Outcomes
TB meningitis carries a guarded prognosis, particularly when diagnosis and treatment are delayed.
Prognostic Indicators:
- Stage at presentation (poor outcomes in stage III)
- Level of consciousness
- Presence of focal deficits
- Drug resistance
Possible Sequelae:
- Cognitive impairment
- Motor deficits (e.g., hemiparesis)
- Vision and hearing loss
- Hydrocephalus requiring long-term shunting
Tuberculosis Meningitis in Special Populations
Pediatric TBM:
- Often presents with nonspecific signs
- Higher risk of neurological damage
- Needs prompt ATT and supportive care
TBM in HIV-Positive Patients:
- Higher incidence of multidrug-resistant TB
- Greater risk of adverse outcomes
- Careful coordination with antiretroviral therapy (ART) initiation to avoid IRIS (immune reconstitution inflammatory syndrome)
Prevention and Public Health Strategies
Primary Prevention:
- Bacillus Calmette–Guérin (BCG) vaccination in infancy
- Early diagnosis and treatment of pulmonary TB
Secondary Prevention:
- Contact tracing and prophylaxis for exposed individuals
- Regular TB screening in high-risk populations
Tuberculosis meningitis remains a life-threatening form of CNS tuberculosis. Early clinical suspicion, timely diagnosis with CSF analysis and neuroimaging, and immediate initiation of antitubercular therapy are essential to improve patient outcomes. Enhanced awareness and public health efforts are pivotal in reducing the burden of TBM, especially in endemic regions and immunocompromised populations.