Trigeminal neuralgia (TN) is a chronic pain disorder characterized by sudden, severe, electric shock-like pain affecting the face. The pain typically follows the distribution of the trigeminal nerve, which is responsible for sensory function in the facial region. Trigeminal neuralgia significantly impairs quality of life and demands a structured diagnostic and therapeutic approach to ensure effective pain control and improved outcomes.
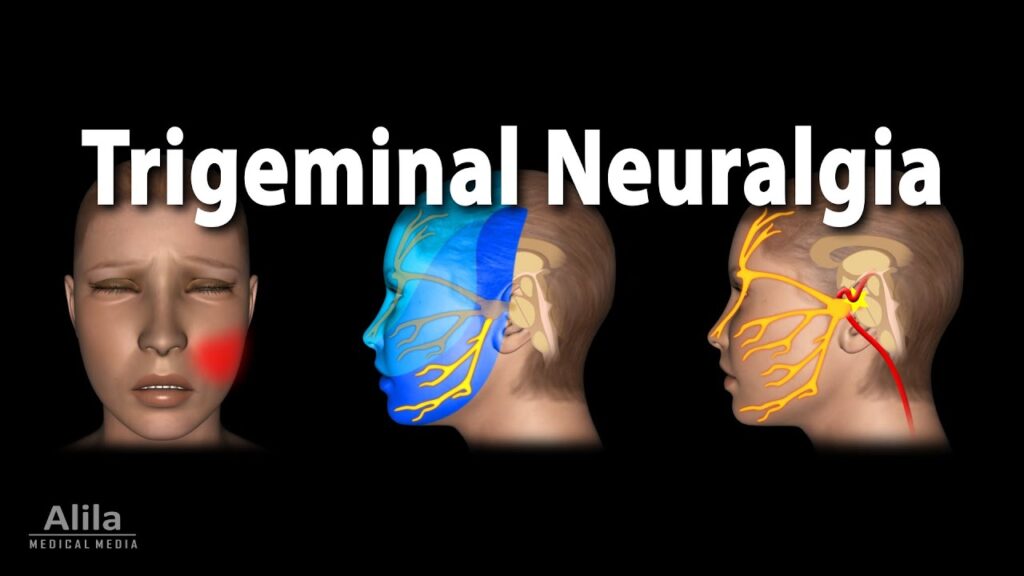
Overview of the Trigeminal Nerve
The trigeminal nerve (cranial nerve V) is the largest cranial nerve and comprises three main branches:
- Ophthalmic (V1) – forehead, scalp, upper eyelid
- Maxillary (V2) – cheek, upper lip, nasal mucosa
- Mandibular (V3) – jaw, lower lip, part of the tongue
These branches transmit sensory signals to the brain, and irritation or compression of any of these divisions can result in trigeminal neuralgia.
Causes and Risk Factors of Trigeminal Neuralgia
Primary (Idiopathic) Trigeminal Neuralgia
Often caused by vascular compression of the trigeminal nerve root, typically by the superior cerebellar artery, leading to demyelination and hyperexcitability.
Secondary Trigeminal Neuralgia
Arises due to an underlying neurological condition or structural lesion, including:
- Multiple sclerosis
- Brainstem infarction
- Tumors (e.g., cerebellopontine angle tumors)
- Arteriovenous malformations
- Trauma or post-surgical nerve damage
Risk Factors
- Age >50 years
- Female sex
- Family history of neuralgia
- Coexisting neurological disorders
Characteristic Symptoms of Trigeminal Neuralgia
- Sudden, paroxysmal facial pain, described as stabbing, electric, or burning
- Pain typically unilateral and localized to V2 or V3
- Duration: seconds to 2 minutes, with symptom-free intervals
- Triggered by minimal stimulation (e.g., talking, brushing teeth, wind exposure)
- No neurological deficits in classical TN
Types of Trigeminal Neuralgia
| Type | Characteristics |
|---|---|
| Classical TN (Type 1) | Sudden, severe pain with trigger zones |
| Atypical TN (Type 2) | Constant aching, burning, or stabbing pain |
| Secondary TN | Associated with underlying lesions or conditions |
Diagnostic Evaluation of Trigeminal Neuralgia
A detailed history and clinical examination remain the cornerstone of diagnosis. Imaging is crucial to exclude secondary causes.
Diagnostic Criteria (ICHD-3)
- Paroxysmal facial pain episodes lasting 1 second to 2 minutes
- Severe intensity with electric shock-like quality
- Occurs in one or more divisions of the trigeminal nerve
- Triggered by innocuous stimuli
- No clinical neurological deficit
Imaging Studies
- MRI with and without contrast: To detect neurovascular compression, tumors, or demyelination
- MRA (Magnetic Resonance Angiography): Useful to visualize vascular loops
- CT Scan: May aid in evaluating bony abnormalities or trauma
Differential Diagnosis
| Condition | Distinguishing Features |
|---|---|
| Cluster headache | Periorbital pain, autonomic symptoms, longer duration |
| Postherpetic neuralgia | History of shingles, persistent burning pain |
| Glossopharyngeal neuralgia | Pain in throat, ear, triggered by swallowing |
| Temporomandibular joint disorder | Jaw clicking, localized pain, worsened by chewing |
Comprehensive Treatment of Trigeminal Neuralgia
Pharmacological Management
First-line therapy focuses on antiepileptic drugs, which stabilize overactive nerve firing.
| Medication | Dosage Range | Notes |
|---|---|---|
| Carbamazepine | 200–1200 mg/day | Most effective, monitor for hyponatremia |
| Oxcarbazepine | 300–1800 mg/day | Better tolerated than carbamazepine |
| Gabapentin | 900–3600 mg/day | Useful in atypical TN |
| Baclofen | 15–80 mg/day | GABA agonist, often used as adjunct |
| Lamotrigine | 100–400 mg/day | Reserved for refractory cases |
Side Effects Monitoring
- Hematological parameters (CBC, liver enzymes)
- Sodium levels (hyponatremia risk)
- Allergic reactions (Stevens-Johnson syndrome with lamotrigine)
Interventional and Surgical Management
Pharmacoresistant cases or those with intolerable side effects require surgical intervention.
1. Microvascular Decompression (MVD)
- Gold standard for classical TN with vascular compression
- Involves repositioning or placing a Teflon pad between vessel and nerve
- High success rate with long-term pain relief
- Requires general anesthesia and carries surgical risks
2. Percutaneous Procedures
Performed under sedation and image guidance:
- Radiofrequency Rhizotomy: Controlled nerve ablation
- Balloon Compression: Mechanical compression of the trigeminal ganglion
- Glycerol Injection: Chemical neurolysis
3. Stereotactic Radiosurgery (Gamma Knife)
- Non-invasive
- Focused radiation targets trigeminal root
- Delayed onset of pain relief (weeks to months)
- Risk of facial numbness
Prognosis and Long-Term Outlook
- Many patients achieve adequate symptom control with medications.
- Recurrence rates vary; surgical interventions offer longer relief but carry procedural risks.
- Ongoing monitoring and lifestyle adjustments improve daily functioning.
Preventive Strategies and Patient Education
- Avoid triggers such as cold air, facial stimulation, and stress.
- Maintain adherence to prescribed medications.
- Educate patients about early signs of recurrence and side effects.
- Psychological support may help in managing the chronic nature of TN.
Frequently Asked Questions:
Q1. Is trigeminal neuralgia curable?
While not curable, it is often manageable with medications or surgery, providing long-term relief.
Q2. What triggers TN attacks?
Common triggers include chewing, brushing teeth, talking, shaving, or even wind exposure.
Q3. Can TN affect both sides of the face?
It typically affects one side. Bilateral TN is rare and often indicates secondary causes like multiple sclerosis.
Q4. How long does TN treatment take to work?
Medications may provide relief within days to weeks; surgical options may offer more sustained benefits.
Q5. What is the best surgical option for TN?
Microvascular decompression is considered the most effective and long-lasting option when vascular compression is confirmed.