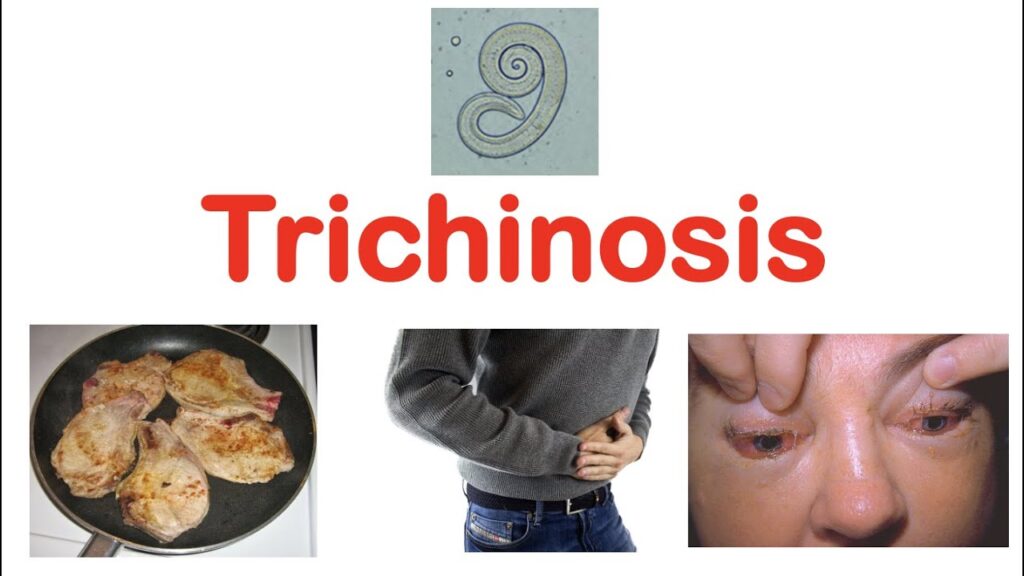
Trichinosis, also known as trichinellosis, is a zoonotic parasitic infection caused by nematodes of the genus Trichinella. It predominantly arises from the consumption of undercooked or raw meat infected with Trichinella larvae, most commonly pork or wild game. The disease poses a significant public health concern worldwide, especially in regions where meat inspection and cooking standards are inadequate.
Understanding Trichinosis: Etiology and Lifecycle of Trichinella
Trichinosis results from ingestion of encysted Trichinella larvae residing in muscle tissues of infected animals. Once consumed, the larvae are released in the small intestine, mature into adult worms, and produce newborn larvae that disseminate hematogenously to skeletal muscles where they encyst.
Epidemiology and Risk Factors for Trichinosis
While trichinosis prevalence has declined in many developed countries due to improved meat inspection and cooking practices, sporadic outbreaks still occur. Risk factors include:
- Consumption of raw or undercooked pork, wild boar, or bear meat.
- Practices such as home slaughter without veterinary inspection.
- Cultural culinary habits involving raw or smoked meats.
- Poor sanitation in animal husbandry allowing for transmission.
Clinical Presentation of Trichinosis: Signs and Symptoms
The clinical spectrum varies depending on parasite load and host immune response, generally categorized into intestinal and systemic phases:
Intestinal Phase
- Occurs 1–2 days post-infection.
- Symptoms: abdominal pain, diarrhea, nausea, vomiting.
- Due to adult worms in intestinal mucosa.
Muscular (Systemic) Phase
- Begins 2–8 weeks post-infection as larvae migrate to muscles.
- Symptoms: myalgia, fever, periorbital edema, conjunctivitis.
- Complications: myocarditis, encephalitis, pneumonia in severe cases.
Chronic Phase
- Rare persistence of muscle inflammation causing prolonged fatigue and weakness.
Diagnostic Modalities for Confirming Trichinosis
Accurate diagnosis requires integrating clinical, laboratory, and epidemiologic data:
- Serologic Tests: ELISA detecting anti-Trichinella antibodies; sensitivity improves after 3-4 weeks post-infection.
- Muscle Biopsy: Identification of encysted larvae in skeletal muscle tissue remains the gold standard.
- Complete Blood Count: Eosinophilia is a hallmark finding.
- Imaging: MRI may reveal muscle inflammation but is nonspecific.
Effective Treatment Protocols for Trichinosis
Prompt antiparasitic therapy is essential to reduce symptom severity and prevent complications:
Antiparasitic Agents
- Albendazole and Mebendazole: First-line treatments; inhibit microtubule synthesis in worms.
- Initiated ideally within 2 weeks of symptom onset.
- Treatment duration typically 10–14 days.
Adjunctive Therapies
- Corticosteroids: Prescribed in moderate to severe cases to alleviate inflammation and systemic symptoms.
- Supportive Care: Analgesics for myalgia, hydration, and monitoring for cardiac or neurologic complications.
Preventive Measures to Reduce Trichinosis Risk
Prevention remains the cornerstone of trichinosis control, emphasizing public health education and food safety:
- Cooking meat to internal temperatures of at least 71°C (160°F) to ensure larval death.
- Freezing pork for extended periods (minimum 20 days at -15°C) reduces larval viability, although this is less effective for wild game.
- Avoiding consumption of raw or undercooked meat products.
- Implementing strict animal husbandry and meat inspection practices.
- Promoting hygienic slaughter and meat processing methods.
Complications and Prognosis of Trichinosis
With timely diagnosis and treatment, most patients experience full recovery. However, severe infections may result in:
- Myocarditis leading to heart failure.
- Central nervous system involvement with encephalitis.
- Respiratory failure due to diaphragmatic muscle involvement.
Mortality is rare but can occur in disseminated or untreated cases.
Comprehensive Management of Trichinosis
Trichinosis demands heightened clinical suspicion in patients presenting with compatible gastrointestinal and muscular symptoms following consumption of at-risk meats. Early serologic testing and initiation of antiparasitic treatment are crucial. Public health interventions and food safety remain vital in preventing transmission and outbreaks.
Frequently Asked Questions:
Q1. How is trichinosis transmitted?
Trichinosis is transmitted by consuming raw or undercooked meat containing Trichinella larvae.
Q2. What are the common symptoms of trichinosis?
Initial symptoms include gastrointestinal upset followed by muscle pain, fever, and swelling around the eyes.
Q3. Which tests confirm trichinosis diagnosis?
Serology for antibodies and muscle biopsy for larvae are the main diagnostic methods.
Q4. What treatments are effective against trichinosis?
Albendazole or mebendazole, combined with corticosteroids for severe cases, form the treatment basis.
Q5. Can trichinosis be prevented?
Yes, by thoroughly cooking meat and ensuring proper meat inspection practices.