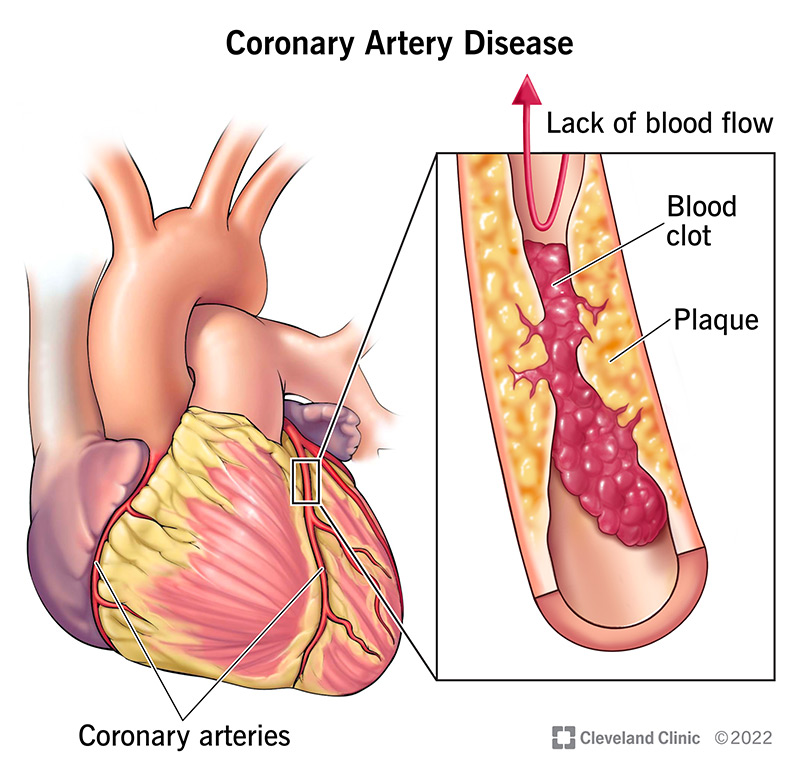
Coronary artery disease (CAD) remains a leading cause of mortality worldwide. Managing its progression requires a multifaceted strategy involving pharmacologic therapy, lifestyle modification, dietary intervention, and sometimes procedural or surgical approaches. By employing evidence-based treatments, we can significantly reduce the burden of atherosclerotic plaque buildup and prevent acute coronary events.
Understanding the Progression of Coronary Artery Disease
CAD is characterized by the gradual accumulation of atherosclerotic plaques in the coronary arteries, leading to reduced blood flow to the heart muscle. Over time, this can result in angina, myocardial infarction, arrhythmias, and heart failure. The progression is driven by modifiable risk factors such as dyslipidemia, hypertension, smoking, diabetes, and sedentary lifestyle.
Pharmacologic Treatments to Slow CAD Progression
Statins (HMG-CoA Reductase Inhibitors)
Statins are the cornerstone therapy for slowing CAD progression.
- Mechanism: Statins lower LDL cholesterol and stabilize existing plaques.
- Examples: Atorvastatin, Rosuvastatin, Simvastatin.
- Clinical Impact: Reduced incidence of myocardial infarction and stroke.
- Guidelines: High-intensity statin therapy recommended for patients with established CAD.
Antiplatelet Therapy
- Aspirin: Inhibits platelet aggregation; lowers risk of thrombosis in narrowed vessels.
- P2Y12 Inhibitors (e.g., clopidogrel): Often used in dual antiplatelet therapy post-PCI or ACS.
ACE Inhibitors and ARBs
- Action: Reduce vascular resistance, blood pressure, and remodeling of the heart.
- Indicated in: Patients with hypertension, diabetes, or heart failure along with CAD.
Beta-Blockers
- Function: Decrease myocardial oxygen demand by reducing heart rate and blood pressure.
- Effectiveness: Particularly beneficial post-myocardial infarction.
SGLT2 Inhibitors and GLP-1 Receptor Agonists
Emerging evidence supports the use of these agents in diabetic patients to reduce cardiovascular events and improve overall heart health.
Lifestyle Modifications: Foundation of Long-Term CAD Management
Dietary Intervention
- Mediterranean Diet: Rich in fruits, vegetables, whole grains, legumes, fish, and olive oil.
- Benefits: Improves lipid profiles, reduces inflammation, and decreases cardiovascular risk.
- Limit Saturated Fats: Avoid red meat, trans fats, and processed foods.
Regular Physical Activity
- Recommendations: At least 150 minutes/week of moderate aerobic activity or 75 minutes/week of vigorous exercise.
- Impact: Enhances endothelial function, reduces blood pressure, and promotes weight control.
Smoking Cessation
- Critical Step: Smoking accelerates atherosclerosis and endothelial dysfunction.
- Tools: Nicotine replacement therapy, behavioral counseling, prescription medications.
Weight Management
- Target: Maintain BMI <25.
- Approach: Calorie control, exercise, and behavioral therapy when needed.
Invasive and Non-Invasive Interventions
Coronary Angioplasty and Stenting
- Use: Alleviate severe blockages, particularly in symptomatic or high-risk patients.
- Benefit: Immediate restoration of blood flow, symptom relief.
Coronary Artery Bypass Grafting (CABG)
- Indications: Multi-vessel disease, diabetes, or left main artery involvement.
- Outcome: Superior long-term outcomes in certain patient populations.
Enhanced External Counterpulsation (EECP)
- Non-invasive therapy: Enhances coronary perfusion and relieves angina in patients unsuitable for revascularization.
Risk Factor Optimization and Monitoring
Blood Pressure Management
- Goal: Maintain BP <130/80 mmHg in patients with CAD.
- Preferred Agents: ACE inhibitors, beta-blockers, calcium channel blockers.
Diabetes Control
- Target HbA1c: <7% in most patients with CAD and diabetes.
- Preferred agents: Metformin, SGLT2 inhibitors, GLP-1 receptor agonists.
Lipid Monitoring
- LDL-C Goal: <70 mg/dL for high-risk individuals.
- Tool: Regular fasting lipid profile.
Integrative and Adjunctive Therapies
Omega-3 Fatty Acids
- Source: Fatty fish, fish oil supplements.
- Effect: Reduce triglycerides, improve endothelial function.
Coenzyme Q10
- Potential Benefit: Antioxidant properties and improved mitochondrial function.
Mindfulness and Stress Reduction
- Impact: Reduces sympathetic activity and stress-induced inflammation.
- Techniques: Meditation, yoga, cognitive behavioral therapy.
Patient Education and Shared Decision-Making
Empowering patients through education improves adherence to treatment and fosters lifestyle transformation. Shared decision-making enables personalization of therapy based on clinical evidence and patient preferences.
A Multidisciplinary Strategy is Key
Slowing the progression of coronary artery disease requires an integrated approach. Pharmacologic therapy, including statins, antiplatelets, ACE inhibitors, and modern diabetic medications, must be combined with lifestyle changes that address diet, exercise, and smoking cessation. Surgical interventions are reserved for advanced cases, but all patients benefit from risk factor monitoring and long-term management.