Transient cerebral ischemia, commonly known as a transient ischemic attack (TIA) or mini-stroke, represents a temporary disruption in the blood supply to the brain. While symptoms typically resolve within minutes to hours, the episode serves as a crucial warning sign of a potential full-blown stroke. Early recognition, prompt evaluation, and targeted management can significantly reduce the risk of subsequent cerebral infarction.
Understanding the Mechanism: What Causes Transient Cerebral Ischemia?
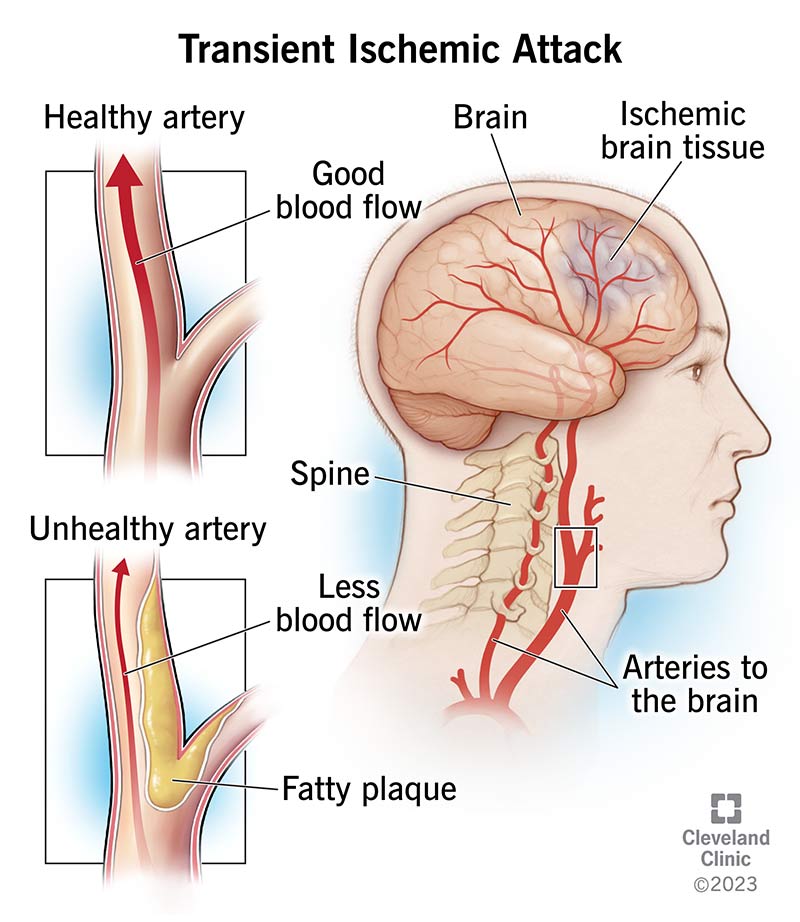
Transient cerebral ischemia occurs when cerebral blood flow is temporarily reduced or obstructed, depriving brain tissue of essential oxygen and nutrients. The ischemia is typically brief enough that it does not result in permanent damage, yet it may indicate underlying vascular pathology.
Common Etiologies
- Atherosclerotic plaque in carotid or cerebral arteries
- Cardioembolic events from atrial fibrillation or heart valve disease
- Arterial dissection
- Small vessel disease
- Hypercoagulable states
Risk Factors Associated with Transient Ischemic Attacks
Numerous factors increase the likelihood of experiencing a TIA:
- Hypertension
- Diabetes mellitus
- Hyperlipidemia
- Smoking
- Obesity
- Sedentary lifestyle
- Atrial fibrillation or other arrhythmias
- Family history of stroke or vascular disease
A comprehensive risk assessment should be conducted to identify modifiable contributors and implement preventative strategies.
Symptoms of Transient Cerebral Ischemia
Transient ischemic attacks present suddenly and often resolve within an hour. However, they may mimic early stroke symptoms and must be treated as a medical emergency.
Typical TIA Symptoms
- Unilateral weakness or numbness (face, arm, leg)
- Speech difficulties (dysarthria or aphasia)
- Vision disturbances (temporary blindness, double vision)
- Dizziness or loss of balance
- Confusion or altered mental state
The acronym FAST (Face drooping, Arm weakness, Speech difficulties, Time to call emergency services) remains a valuable tool in public awareness.
Diagnosis and Evaluation of Transient Cerebral Ischemia
Immediate Clinical Assessment
Following a suspected TIA, evaluation should begin urgently to identify the source and implement secondary prevention.
Key Diagnostic Procedures
- Neurological examination
- Brain imaging: MRI with diffusion-weighted imaging is preferred to detect small infarcts.
- Carotid ultrasound: Evaluates for carotid artery stenosis.
- Echocardiogram: Assesses for cardiac sources of emboli.
- Electrocardiogram (ECG): Detects atrial fibrillation or other arrhythmias.
- Blood tests: Glucose, lipid profile, coagulation panel, complete blood count.
ABCD2 Score: Predicting Stroke Risk After a TIA
The ABCD2 scoring system helps estimate short-term stroke risk following a transient ischemic attack:
| Criteria | Points |
|---|---|
| Age ≥ 60 | 1 |
| Blood Pressure ≥ 140/90 mmHg | 1 |
| Clinical Features: Unilateral Weakness | 2 |
| Clinical Features: Speech Disturbance without Weakness | 1 |
| Duration ≥ 60 minutes | 2 |
| Duration 10–59 minutes | 1 |
| Diabetes Mellitus | 1 |
Total Score Interpretation:
- 0–3: Low risk
- 4–5: Moderate risk
- 6–7: High risk
Treatment Strategies for Transient Cerebral Ischemia
Acute Management
Although symptoms resolve, every TIA should be treated as an emergency.
- Hospital observation (especially for high ABCD2 score)
- Antiplatelet therapy (aspirin, clopidogrel)
- Anticoagulation (if atrial fibrillation is confirmed)
- Statin therapy for lipid control
- Blood pressure management
Surgical and Interventional Options
- Carotid endarterectomy: Indicated for patients with significant carotid artery stenosis.
- Carotid artery stenting: Considered in select high-risk patients.
Preventing Recurrence and Long-Term Stroke Risk Reduction
Prevention focuses on lifestyle modification and medical management to reduce the risk of a future stroke.
Key Preventive Measures
- Smoking cessation
- Dietary changes (low saturated fats, increased fiber and vegetables)
- Regular physical activity
- Weight management
- Control of diabetes and hypertension
- Adherence to prescribed antiplatelet/anticoagulant therapy
Routine follow-up with neurology and cardiology specialists enhances long-term outcomes.
Transient Cerebral Ischemia in Special Populations
Elderly Patients
Often have comorbidities that elevate risk and complicate management; careful adjustment of medications is crucial.
Women
May have under-recognized symptoms; higher stroke risk in the presence of hormone therapy or migraine with aura.
Young Adults
Often due to less common causes such as arterial dissection, drug abuse, or thrombophilia; require thorough evaluation.
Frequently Asked Questions:
How serious is a transient cerebral ischemia?
Though symptoms resolve quickly, it is a warning sign of an impending stroke. Without treatment, the risk of stroke within 48 hours can be high.
Can TIA cause permanent damage?
Generally, no. However, repeated events or lack of timely care can lead to cumulative neurological injury.
Is hospitalization necessary after a TIA?
Yes, especially for high-risk individuals. Prompt evaluation helps prevent more severe outcomes.
What is the difference between a TIA and a stroke?
A TIA resolves completely without lasting damage, while a stroke causes permanent brain injury.
How soon after a TIA should treatment begin?
Immediately. The highest risk of stroke is within the first 48 hours after a TIA.
Transient cerebral ischemia, or TIA, serves as a vital early warning signal for potentially devastating cerebrovascular events. Timely recognition, accurate diagnosis, and immediate treatment can prevent progression to permanent brain damage. Through vigilant risk factor management, patient education, and targeted therapy, we can significantly reduce the global burden of stroke.

