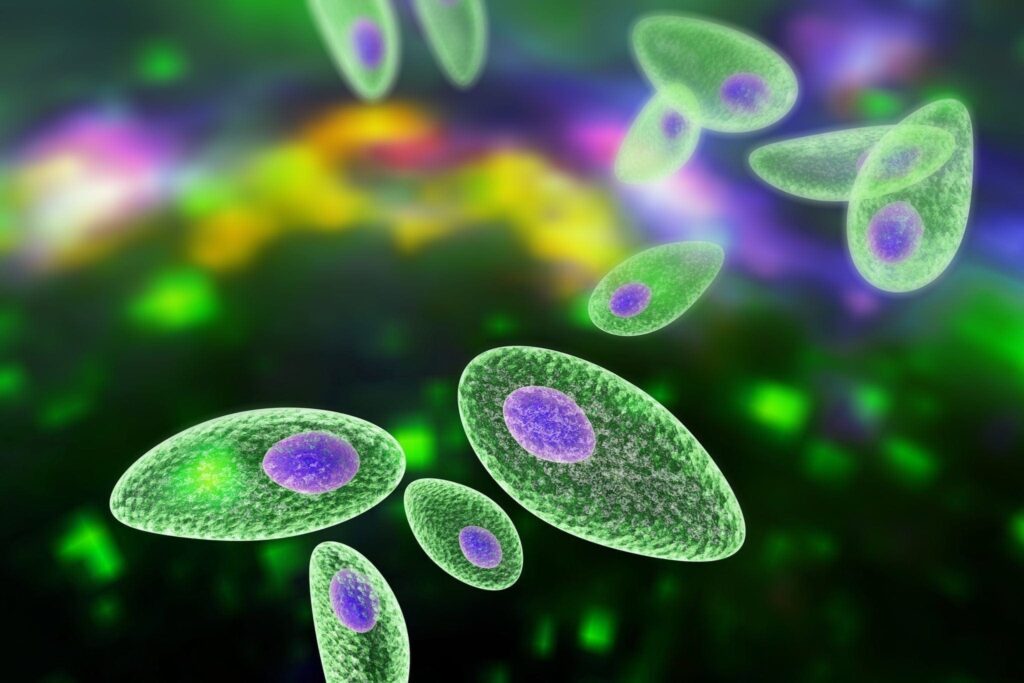
Toxoplasmosis is an infectious disease caused by Toxoplasma gondii, a protozoan parasite of global concern. This pathogen affects both humans and warm-blooded animals and is primarily transmitted through ingestion of oocysts or tissue cysts. While the majority of infected individuals remain asymptomatic, toxoplasmosis poses severe risks to immunocompromised individuals and fetuses when transmitted during pregnancy.
Primary Modes of Transmission
- Ingestion of Contaminated Food or Water: Raw or undercooked meat containing tissue cysts is a primary source of infection.
- Contact with Feline Feces: Exposure to cat litter or soil contaminated with oocysts is a significant risk.
- Congenital Transmission: Infected mothers can transmit the parasite to the fetus during pregnancy.
- Organ Transplants or Blood Transfusions: Rare, but documented cases exist.
- Unpasteurized Dairy Products: May harbor viable organisms in certain cases.
Symptoms of Toxoplasmosis
Toxoplasmosis manifests in various clinical forms, ranging from asymptomatic to severe systemic involvement.
Acute Toxoplasmosis
In immunocompetent individuals, symptoms, if any, may include:
- Mild fever
- Lymphadenopathy (especially cervical nodes)
- Fatigue
- Muscle aches
- Headache
Ocular Toxoplasmosis
When the parasite localizes in the retina:
- Blurred vision
- Floaters
- Eye pain and redness
- Potential permanent vision loss
Congenital Toxoplasmosis
Infection during pregnancy can result in:
- Miscarriage or stillbirth
- Hydrocephalus
- Intracranial calcifications
- Chorioretinitis
- Developmental delays
Toxoplasmosis in Immunocompromised Individuals
Individuals with HIV/AIDS, cancer, or on immunosuppressive therapy are at risk for:
- Encephalitis
- Seizures
- Confusion and memory loss
- Ataxia
- Coma in severe cases
Diagnosis of Toxoplasmosis
Accurate diagnosis requires serological, molecular, and imaging techniques.
Serological Testing
- IgM and IgG Antibody Testing: Helps determine recent or past infection.
- Avidity Testing: Differentiates recent infections from older ones by evaluating IgG avidity.
Molecular Testing
- Polymerase Chain Reaction (PCR): Detects T. gondii DNA in blood, amniotic fluid, or cerebrospinal fluid, especially useful in congenital and CNS cases.
Imaging Studies
- CT or MRI Scans: Useful in detecting toxoplasmic encephalitis lesions in immunocompromised patients.
- Ophthalmologic Exam: Identifies retinal lesions characteristic of ocular toxoplasmosis.
Treatment of Toxoplasmosis
Treatment varies based on clinical form and immune status.
Immunocompetent Individuals
Treatment may not be required for mild, self-limiting cases. If symptoms persist:
- Pyrimethamine + Sulfadiazine + Leucovorin: Standard regimen for 4–6 weeks.
Pregnant Women
- Spiramycin: Used during the first trimester to reduce transmission risk.
- Pyrimethamine-Sulfadiazine: Applied later in pregnancy if fetal infection is confirmed.
Immunocompromised Patients
- Lifelong maintenance therapy may be required after initial treatment.
- Close monitoring of CD4 counts and imaging recommended.
Ocular Infections
- Corticosteroids combined with antiparasitic drugs are administered under ophthalmological supervision.
Complications and Long-Term Effects
Toxoplasmosis can lead to severe complications in specific populations:
- Neurological damage from encephalitis or congenital infection
- Visual impairment or blindness
- Developmental delays in infants
- Chronic active infection in immunocompromised individuals
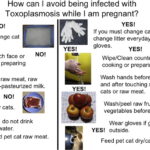
Preventive Measures Against Toxoplasmosis
Preventive strategies are crucial to reduce the burden of this globally prevalent infection.
Food Safety Practices
- Cook meat to an internal temperature of at least 67°C (153°F).
- Wash fruits and vegetables thoroughly.
- Avoid unpasteurized milk products.
Pet Hygiene
- Avoid handling cat litter during pregnancy.
- Clean litter boxes daily using gloves and hot water.
- Prevent cats from hunting and feeding on raw meat.
Environmental Hygiene
- Use gloves while gardening.
- Wash hands thoroughly after soil contact.
- Keep sandboxes covered when not in use.
Special Considerations for Pregnant Women
- Regular prenatal screening in endemic areas.
- Avoid high-risk foods and contact with cat litter.
- Immediate testing and treatment if exposure is suspected.
Epidemiology and Global Burden
Toxoplasmosis has a widespread global distribution:
- Approximately 30–50% of the world’s population has been exposed.
- Seroprevalence varies by region, with higher rates in tropical and underdeveloped areas.
- In the United States, 11–15% of individuals aged 6–49 show serological evidence.
- Leading cause of foodborne death-related hospitalizations according to CDC data.
Toxoplasmosis, though often underestimated, carries serious implications for public health, particularly among vulnerable populations. Its complex transmission cycle, diverse clinical presentations, and potential for congenital or neurological damage necessitate vigilance in diagnosis, timely treatment, and robust preventive strategies. By adhering to safe food practices, maintaining environmental hygiene, and ensuring regular medical monitoring, we can substantially mitigate the risks associated with this parasitic disease.
Frequently Asked Questions
What is toxoplasmosis caused by?
Toxoplasmosis is caused by the protozoan parasite Toxoplasma gondii, transmitted through contaminated food, water, or contact with cat feces.
Can toxoplasmosis go away on its own?
In healthy individuals, the infection may resolve without treatment. However, medical intervention is essential for pregnant women and immunocompromised persons.
Is toxoplasmosis dangerous during pregnancy?
Yes, it can lead to miscarriage, stillbirth, or severe congenital abnormalities if the fetus becomes infected.
Can I get toxoplasmosis from my cat?
Yes, if you handle contaminated litter or soil with oocysts. However, direct contact with cats rarely transmits the disease.
How can I prevent toxoplasmosis?
Cook meat thoroughly, wash hands and vegetables, and avoid handling cat litter during pregnancy. Regular screening is also advisable in high-risk individuals.