Phenobarbital is a long-acting barbiturate widely used in the treatment of epilepsy, status epilepticus, and certain withdrawal syndromes. It exerts its effect by enhancing the inhibitory actions of gamma-aminobutyric acid (GABA) at GABA-A receptors, promoting sedation, anticonvulsant activity, and hypnosis.
Phenobarbital is favored for its effectiveness and long half-life, which allows for once-daily dosing. However, due to its narrow therapeutic index, monitoring of serum levels is critical. Toxicity can occur with relatively small dosage changes or accumulation over time.
Therapeutic and Toxic Phenobarbital Serum Levels
Therapeutic Range
- Adults and Children: 15–40 mcg/mL (65–172 µmol/L)
- The target range for seizure control is typically 20–40 mcg/mL.
Toxic Serum Levels
- Mild Toxicity: >40 mcg/mL
- Moderate to Severe Toxicity: >60 mcg/mL
- Potentially Fatal: >80–100 mcg/mL
Toxic levels often result from intentional overdose, impaired hepatic metabolism, renal insufficiency, or drug interactions that inhibit phenobarbital clearance.
Causes of Elevated Phenobarbital Serum Levels
1. Intentional or Accidental Overdose
- Common in suicide attempts or medication errors
- Symptoms can present after ingestion of more than 10 mg/kg in non-tolerant individuals
2. Drug Interactions
Phenobarbital is both a substrate and an inducer of CYP450 enzymes. Inhibitors such as valproic acid can increase serum concentrations by reducing clearance.
3. Impaired Hepatic or Renal Function
Since phenobarbital is primarily metabolized in the liver and excreted renally, dysfunction in either system can lead to accumulation and toxicity.
4. Chronic Use with Dose Escalation
Over time, patients may develop tolerance to the sedative effects, prompting dosage increases that risk surpassing the therapeutic window.
Symptoms of Phenobarbital Toxicity
Toxicity affects the central nervous system, respiratory function, and cardiovascular stability. The severity correlates with serum concentration.
Neurological Signs:
- Drowsiness progressing to stupor and coma
- Ataxia, dysarthria, and vertigo
- Slurred speech, nystagmus
- Hyporeflexia and cognitive impairment
- Seizures (paradoxical, at very high levels)
Respiratory Effects:
- Respiratory depression
- Hypoventilation
- Hypoxia due to CNS depression
Cardiovascular Effects:
- Hypotension
- Bradycardia
- Shock in severe cases
Other Symptoms:
- Hypothermia
- Blistering due to prolonged immobility
- Rhabdomyolysis and renal failure in prolonged coma
Diagnostic Approach to Phenobarbital Toxicity
A high index of suspicion and a thorough clinical history are essential in diagnosis. Confirmatory testing and differential diagnosis follow.
1. Serum Phenobarbital Level Testing
- Performed via immunoassay or gas chromatography
- Essential for confirming toxic levels and guiding treatment
2. Arterial Blood Gas (ABG)
- Identifies respiratory acidosis due to hypoventilation
3. Electrolytes and Renal Function Panel
- Identifies renal failure or electrolyte imbalances
4. Liver Function Tests
- Assesses hepatic clearance capacity
5. ECG
- Rules out bradyarrhythmias or conduction abnormalities
Management of Toxic Phenobarbital Levels
Management depends on the severity of toxicity and involves supportive care, enhanced elimination, and monitoring.
1. Immediate Supportive Care
- Airway management: Intubation if GCS < 8 or signs of respiratory depression
- Oxygen supplementation and ventilation support
- IV fluid resuscitation: For hypotension and renal perfusion
2. Gastrointestinal Decontamination
- Activated Charcoal: If patient presents within 1–2 hours post-ingestion and airway is protected
- Repeated-dose Activated Charcoal (MDAC): Enhances elimination by interrupting enterohepatic circulation
3. Enhanced Elimination
- Hemodialysis: Not routinely used but may be indicated in severe toxicity or renal failure
- Urinary Alkalinization: Increases renal clearance; rarely used today due to limited efficacy
4. Monitoring and Observation
- Serum levels every 6–12 hours until within therapeutic range
- Cardiac monitoring, vital signs, and neurological status hourly in ICU settings
- Liver and renal function daily or as clinically indicated
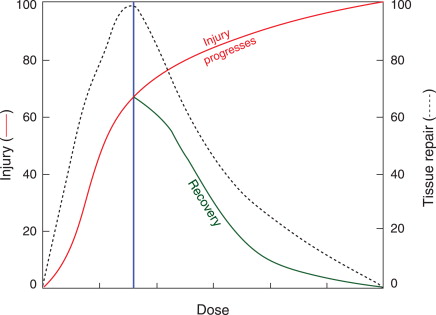
Prognosis and Recovery
Most patients recover fully with early intervention and intensive supportive care. The half-life of phenobarbital ranges from 53 to 140 hours in overdose cases, meaning patients may require prolonged hospitalization. Complications can include aspiration pneumonia, prolonged mechanical ventilation, and pressure injuries.
Prognostic Factors:
- Serum levels >100 mcg/mL: Associated with increased mortality
- Delayed treatment: Worsens outcome
- Comorbidities: Hepatic, renal, or respiratory compromise
Prevention of Toxic Phenobarbital Serum Levels
1. Therapeutic Drug Monitoring (TDM)
Routine serum level checks in patients on long-term phenobarbital therapy prevent accumulation and toxicity.
2. Medication Reconciliation
Regular reviews of drug regimens reduce the risk of harmful interactions, especially in polypharmacy cases.
3. Patient Education
Instruct patients on signs of toxicity, adherence to prescribed dosages, and the importance of follow-up visits.
4. Pharmacogenomics
Emerging research supports the potential role of genetic testing in predicting metabolic variations in phenobarbital clearance.
Toxic phenobarbital serum levels represent a serious clinical condition requiring immediate recognition, accurate serum level assessment, and targeted intervention. Given its narrow therapeutic index and long half-life, phenobarbital demands vigilant monitoring to prevent toxicity. Comprehensive care, from emergency response to long-term follow-up, is essential for favorable outcomes.

