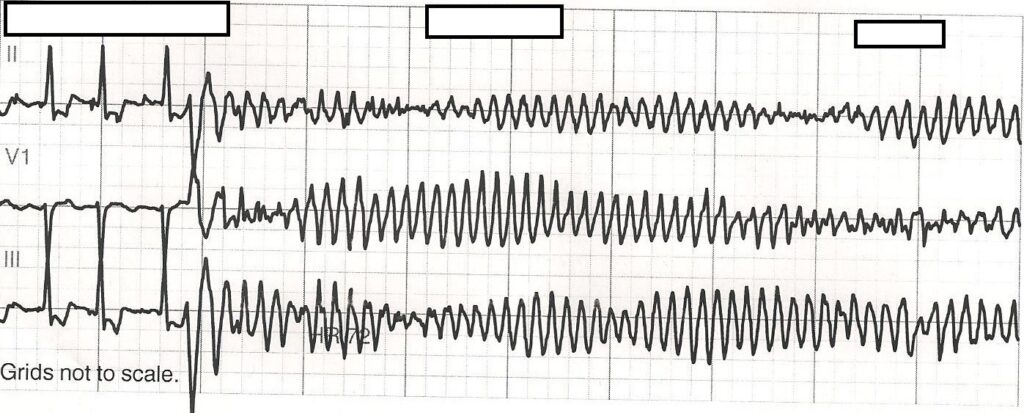
Torsades de Pointes (TdP), a French term meaning “twisting of the points,” is a distinctive form of polymorphic ventricular tachycardia (VT) associated with a prolonged QT interval on electrocardiogram (ECG). This arrhythmia is characterized by rapid, irregular QRS complexes that appear to twist around the isoelectric line and can progress to ventricular fibrillation, leading to sudden cardiac death if not promptly managed.
Etiology: Underlying Causes of Torsades de Pointes
1. Congenital Long QT Syndrome
Inherited channelopathies, such as Romano-Ward and Jervell and Lange-Nielsen syndromes, impair repolarization due to dysfunctional ion channels.
2. Acquired QT Prolongation
The majority of TdP cases arise from acquired factors that prolong the QT interval.
Common Acquired Causes:
- Medications: Antiarrhythmics (e.g., amiodarone, sotalol), antibiotics (e.g., erythromycin, levofloxacin), antipsychotics (e.g., haloperidol), antidepressants (e.g., citalopram)
- Electrolyte Abnormalities: Hypokalemia, hypomagnesemia, hypocalcemia
- Bradyarrhythmias: Especially complete heart block or sinus node dysfunction
- Structural Heart Disease: Left ventricular hypertrophy, myocardial infarction
- Drug Interactions: Especially involving CYP450 inhibitors that increase serum drug levels
3. Genetic and Environmental Interactions
Polymorphisms in ion channel genes may increase susceptibility to acquired QT prolongation.
Pathophysiology: Mechanism Behind Torsades de Pointes
Torsades de Pointes arises due to early afterdepolarizations (EADs) during the repolarization phase of the cardiac action potential. QT prolongation predisposes to these EADs, which can trigger ventricular tachyarrhythmias through reentrant or focal mechanisms.
Clinical Presentation: Recognizing Symptoms
Patients with TdP may present with a range of clinical manifestations, often related to transient reductions in cardiac output due to the rapid ventricular rate.
Key Symptoms Include:
- Palpitations
- Dizziness or lightheadedness
- Syncope or near-syncope
- Seizure-like activity (due to cerebral hypoperfusion)
- Sudden cardiac arrest (in cases of sustained TdP or degeneration to VF)
Symptoms may be preceded by a prodrome of fatigue, nausea, or chest discomfort, especially in drug-induced cases.
Electrocardiographic Characteristics of Torsades de Pointes
The diagnosis of TdP is established through characteristic ECG findings:
- QT Prolongation: QTc > 470 ms in men and > 480 ms in women
- Polymorphic VT Pattern: Twisting morphology around the baseline
- Cycle Length Variation: Progressive lengthening and shortening of R-R intervals
- Pause-Dependent Onset: Often initiated by a long-short R-R sequence
- Biphasic or Triphasic QRS Complexes: Irregular amplitude and axis
Diagnostic Evaluation
1. Electrocardiography (ECG)
Baseline and dynamic ECG monitoring is essential to detect QT prolongation and ventricular arrhythmias.
2. Serum Electrolyte Panel
Evaluation for hypokalemia, hypomagnesemia, and hypocalcemia.
3. Medication Review
Identify QT-prolonging drugs and potential drug interactions.
4. Genetic Testing
Recommended for individuals with recurrent TdP without identifiable causes, or with a family history of sudden cardiac death.
5. Holter Monitoring
For intermittent or asymptomatic episodes.
Management and Treatment of Torsades de Pointes
1. Immediate Stabilization
- Unstable TdP (loss of consciousness or pulseless): Immediate defibrillation
- Stable TdP (conscious with symptoms): Focus on magnesium and QT normalization
2. Pharmacologic Interventions
- Magnesium Sulfate: First-line treatment even if serum magnesium is normal; 2g IV over 10-15 minutes, repeat as needed
- Potassium Repletion: Aim for K⁺ > 4.5 mmol/L
- Lidocaine or Mexiletine: Class IB antiarrhythmics in congenital long QT
- Isoproterenol: In bradycardia-induced TdP; increases heart rate and shortens QT
3. Temporary Pacing
Overdrive pacing at 90-110 bpm may be necessary to prevent recurrence by reducing QT interval and preventing pauses.
4. Withdrawal of Offending Agents
Discontinue all QT-prolonging drugs immediately.
5. Long-Term Management
- Implantable Cardioverter-Defibrillator (ICD): For high-risk or recurrent cases
- Beta-Blockers: Especially in congenital long QT syndrome
- Lifestyle Modification: Avoidance of QT-prolonging drugs, electrolyte imbalance, and strenuous exercise
Prevention Strategies for Torsades de Pointes
- Routine ECG screening for patients on known QT-prolonging drugs
- Monitoring electrolyte levels in hospitalized or critically ill patients
- Avoidance of polypharmacy, especially with CYP450 interactions
- Genetic counseling for families with congenital long QT syndrome
Prognosis and Outcomes
With early recognition and appropriate management, TdP is often reversible. However, delays in diagnosis or treatment significantly increase the risk of degeneration to ventricular fibrillation and sudden death. Patients with congenital long QT syndrome may require lifelong monitoring and intervention.
Frequently Asked Questions:
Q1: What is the most common cause of torsades de pointes?
Acquired QT prolongation due to medications and electrolyte disturbances is the leading cause.
Q2: How is torsades de pointes different from regular ventricular tachycardia?
TdP is a polymorphic VT with QT prolongation, while regular VT is often monomorphic and not linked to QT changes.
Q3: Why is magnesium used in torsades de pointes?
Magnesium stabilizes cardiac ion channels and suppresses early afterdepolarizations.
Q4: Can torsades de pointes occur without symptoms?
Yes, some episodes are asymptomatic and only detected on ECG monitoring.
Q5: Is torsades de pointes fatal?
If untreated, it can degenerate into ventricular fibrillation and result in sudden cardiac death.
Torsades de Pointes is a critical cardiac arrhythmia with well-defined clinical and electrocardiographic features. Prompt diagnosis, correction of underlying causes, and evidence-based treatment are vital to prevent recurrence and fatal outcomes. As medical professionals, we emphasize comprehensive risk assessment, cautious use of QT-prolonging agents, and vigilant ECG monitoring in vulnerable populations.

