Toothache, also known as odontalgia, is one of the most common forms of oral pain affecting individuals of all ages. It ranges from mild discomfort to intense, debilitating pain and can significantly impact one’s daily function. A toothache typically signals an underlying dental issue that requires prompt evaluation and treatment.

Primary Causes of Toothache
Tooth pain arises when the innermost layer of the tooth, the pulp, becomes inflamed or irritated. The pulp contains nerves and blood vessels that react strongly to injury, decay, or infection.
1. Dental Caries (Cavities)
Cavities are caused by bacterial acids eroding the enamel and dentin, eventually reaching the pulp. Pain may present as sensitivity or a sharp ache.
2. Pulpitis
Pulpitis is the inflammation of the dental pulp due to untreated cavities or trauma. It may be reversible or irreversible:
- Reversible pulpitis: Mild pain that subsides after stimulus removal.
- Irreversible pulpitis: Persistent, throbbing pain that often worsens at night.
3. Dental Abscess
A dental abscess is a pus-filled infection at the root tip or gums. It causes severe, localized pain, swelling, and systemic symptoms such as fever.
4. Cracked Tooth Syndrome
Microscopic fractures in the tooth structure can lead to pain on biting or exposure to temperature changes.
5. Impacted Teeth
Most commonly affecting wisdom teeth, impaction causes pain from pressure, inflammation, or adjacent tooth damage.
6. Periodontal Disease
Advanced gum disease causes inflammation, gum recession, and damage to the supporting structures of the teeth, often resulting in dull, persistent pain.
7. Bruxism
Grinding or clenching of teeth leads to tooth and jaw pain, often associated with stress or misaligned bites.
Toothache Symptomatology and Pain Types
Toothaches vary based on cause, location, and severity. Symptoms may include:
- Sharp or throbbing pain
- Pain upon chewing or biting
- Temperature sensitivity (hot or cold)
- Swelling around the tooth or jaw
- Red, bleeding gums
- Fever or headache (in infections)
- Foul taste or odor from the mouth
Diagnostic Process for Toothache
A precise diagnosis is essential for effective treatment. The evaluation includes:
1. Clinical Examination
Dentists inspect for cavities, gum recession, fractures, and signs of abscesses.
2. Radiographic Imaging
Dental X-rays reveal:
- Deep caries
- Bone loss from periodontitis
- Abscess formation
- Cracks and fractures
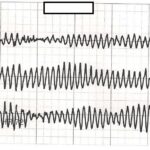
3. Pulp Vitality Tests
Cold, heat, and electric pulp tests determine if the pulp is alive or necrotic.
4. Percussion and Palpation
Tapping the affected tooth or applying pressure helps localize pain and inflammation.
Treatment Options for Toothache
Treatment depends on the underlying cause and may include conservative or invasive interventions.
1. Cavity Filling
In early-stage decay, removing the carious tissue and restoring the tooth with a filling material alleviates pain.
2. Root Canal Therapy
For irreversible pulpitis or abscesses, root canal therapy removes infected pulp, disinfects the canals, and seals the tooth.
3. Tooth Extraction
Severely damaged or impacted teeth that cannot be restored are extracted to eliminate the source of pain.
4. Periodontal Therapy
Scaling and root planing, along with antibiotics, treat pain due to gum infections.
5. Occlusal Adjustments
Night guards and bite corrections are used for bruxism-related pain.
6. Pain Management
- Analgesics: Ibuprofen or acetaminophen for mild to moderate pain.
- Antibiotics: Prescribed only for infections (e.g., abscesses).
- Topical agents: Benzocaine for temporary relief.
Home Remedies and Temporary Relief
Though professional care is essential, temporary relief can be achieved through:
- Cold compress on the cheek
- Saltwater rinses to reduce swelling
- Clove oil for natural analgesic effects
- Over-the-counter pain relievers
These remedies should not replace clinical evaluation and treatment.
Prevention of Toothache
Preventive care remains the most effective approach to avoid dental pain:
- Brush twice daily with fluoride toothpaste
- Floss regularly to prevent interproximal decay
- Avoid sugary foods and drinks
- Attend biannual dental checkups
- Wear protective gear during sports
- Use a mouthguard if bruxism is present
When to See a Dentist
Immediate dental consultation is advised if:
- Pain persists for more than 48 hours
- There is visible swelling or pus
- You experience fever or malaise
- Difficulty in swallowing or breathing occurs
- Pain worsens at night or radiates to the jaw, ear, or neck
Complications of Untreated Toothache
Neglecting a toothache can lead to:
- Spread of infection to facial bones or sinuses
- Formation of deep abscesses
- Loss of the affected tooth
- Sepsis in rare, severe cases
Frequently Asked Questions:
Q1: What is the most common cause of a toothache?
Dental caries (cavities) are the leading cause of tooth pain due to pulp exposure.
Q2: Can a toothache go away on its own?
Mild pain may subside, but underlying issues typically require professional treatment.
Q3: What helps a toothache at night?
Elevating the head, using cold compresses, and taking pain relievers can provide temporary relief.
Q4: Can a sinus infection cause toothache?
Yes, maxillary sinus infections can cause referred pain to the upper molars.
Q5: Is it okay to apply heat to a toothache?
Cold compresses are generally recommended. Heat may worsen infection-related pain.
Toothache is not merely a minor discomfort but a critical symptom that often signals deeper oral health issues. Timely diagnosis, appropriate treatment, and preventive care are essential to alleviate pain, restore dental function, and maintain long-term oral health. As advocates of dental well-being, we emphasize the importance of seeking professional care at the first sign of discomfort.