Haemophilus influenzae is a Gram-negative coccobacillus commonly found in the upper respiratory tract. Though traditionally associated with pneumonia and meningitis, it can also colonize the oropharynx and cause tonsillopharyngitis, particularly in immunocompromised individuals, young children, and those with underlying respiratory conditions.
Among its various serotypes, type b (Hib) is historically the most virulent. However, non-typeable strains (NTHi) are now more frequently implicated in localized infections such as tonsillitis, otitis media, and sinusitis.

Pathogenesis: How Haemophilus influenzae Causes Tonsillar Inflammation
H. influenzae adheres to the epithelial surfaces of the oropharynx using pili and outer membrane proteins. Once colonization is established, the bacteria evade immune responses through mechanisms such as:
- IgA protease production, which degrades mucosal antibodies
- Polysaccharide capsule (in typeable strains), allowing resistance to phagocytosis
- Biofilm formation, especially by non-typeable strains, promoting chronic inflammation
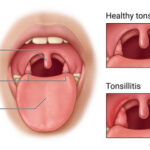
This pathogenic activity results in erythema, swelling, and painful inflammation of the tonsils, often accompanied by purulent exudate.
Epidemiology: Who Is at Risk for H. influenzae Tonsillitis?
High-Risk Populations:
- Children under 5 (especially unvaccinated against Hib)
- Elderly adults
- Individuals with chronic obstructive pulmonary disease (COPD)
- Patients with weakened immune systems (e.g., HIV, diabetes)
- People in close-contact settings (e.g., daycare, prisons)
Though rare in healthy adults, cases of H. influenzae tonsillitis can occur following viral infections, which compromise mucosal defenses and facilitate bacterial superinfection.
Clinical Presentation of Tonsillitis Caused by Haemophilus influenzae
Typical Symptoms:
- Severe sore throat, often unilateral
- Tonsillar hypertrophy with erythema and pus
- Dysphagia (painful swallowing)
- High fever
- Cervical lymphadenopathy
- Fatigue and malaise
In severe cases, symptoms may mimic peritonsillar abscess, with trismus, uvular deviation, and muffled voice.
Differential Diagnosis: Distinguishing from Other Causes
It is critical to differentiate Haemophilus influenzae tonsillitis from other bacterial and viral infections:
| Condition | Key Differentiator |
|---|---|
| Group A Strep tonsillitis | Sudden onset, strawberry tongue, no cough |
| Epstein-Barr Virus | Splenomegaly, generalized lymphadenopathy |
| Diphtheria | Gray pseudomembrane, systemic toxicity |
| Adenoviral pharyngitis | Conjunctivitis, mild systemic symptoms |
Precise microbial identification is essential for proper treatment.
Diagnostic Workup for Haemophilus influenzae Tonsillitis
Clinical Evaluation
- Oropharyngeal examination revealing inflamed tonsils with purulent exudate
- Palpation of tender cervical nodes
Laboratory Tests
- Throat culture on chocolate agar (requires X and V factors for growth)
- Polymerase Chain Reaction (PCR) for species confirmation
- Gram stain showing small Gram-negative coccobacilli
- Blood culture in systemic cases or suspected sepsis
- C-reactive protein (CRP) and white blood cell (WBC) count for inflammation assessment
Prompt identification guides effective antibiotic therapy and reduces complications.
Treatment Strategies for Haemophilus influenzae-Induced Tonsillitis
First-Line Antibiotics
| Antibiotic | Dosage & Duration | Notes |
|---|---|---|
| Amoxicillin-clavulanate | 875 mg twice daily for 7–10 days | Effective against β-lactamase-producing strains |
| Cefuroxime axetil | 250–500 mg twice daily | Useful in penicillin allergy (non-anaphylactic) |
| Ceftriaxone (IM/IV) | For severe infections | Often used in hospitalized patients |
| Azithromycin | 500 mg day 1, 250 mg x 4 days | Macrolide alternative |
Note: Resistance to ampicillin is common due to β-lactamase production, necessitating use of β-lactamase inhibitor combinations.
Supportive Care
- Adequate hydration
- Analgesics and antipyretics
- Saltwater gargles
- Nutritional support in case of poor oral intake
Preventive Measures: Reducing the Risk of H. influenzae Tonsillitis
1. Vaccination
- Hib vaccine is highly effective in preventing invasive type b infections.
- Recommended as part of routine childhood immunization schedule.
2. Infection Control
- Avoid close contact with infected individuals
- Adherence to hand hygiene protocols
- Timely treatment of upper respiratory infections to prevent secondary bacterial colonization
3. Prophylactic Antibiotics
- Reserved for high-risk close contacts in outbreak settings (e.g., rifampin prophylaxis)
Complications of Unmanaged H. influenzae Tonsillitis
If untreated or misdiagnosed, H. influenzae tonsillitis may lead to:
- Peritonsillar abscess
- Otitis media
- Sinusitis
- Sepsis
- Airway obstruction
- Rarely, bacteremic spread to CNS or lungs
These complications highlight the need for early detection and appropriate therapy.
Tonsillectomy and Surgical Considerations
While most infections resolve with medication, surgical intervention may be warranted in cases of:
- Recurrent bacterial tonsillitis unresponsive to antibiotics
- Tonsillar hypertrophy causing airway obstruction
- Chronic carrier state
Tonsillectomy eliminates the nidus of infection and significantly improves quality of life in recurrent cases.
Prognosis and Recovery
With prompt antibiotic therapy, the prognosis for H. influenzae tonsillitis is excellent. Most patients experience symptom resolution within 5 to 7 days. Delayed treatment or resistance may prolong illness, emphasizing the importance of targeted antimicrobial selection.
Frequently Asked Questions
Can Haemophilus influenzae cause sore throat without tonsillitis?
Yes, it may cause pharyngitis without tonsillar involvement, especially in adults with chronic lung disease.
Is H. influenzae contagious?
Yes, it spreads through respiratory droplets. Carriers may remain asymptomatic yet transmit the pathogen.
Can tonsillitis recur after treatment?
Reinfection is possible, especially with non-typeable strains, or in immunocompromised hosts.
What if antibiotics don’t work?
A follow-up culture and antibiotic susceptibility testing are needed to adjust treatment.
Does the Hib vaccine prevent all H. influenzae infections?
No, the Hib vaccine targets type b only. Non-typeable strains can still cause infections, including tonsillitis.
Effective Management of Haemophilus influenzae Tonsillitis
Tonsillitis due to Haemophilus influenzae is an important yet often overlooked form of bacterial pharyngotonsillitis. Through vigilant clinical assessment, timely laboratory diagnosis, and evidence-based antibiotic therapy, outcomes are generally favorable. Preventive strategies, including immunization and infection control, further reduce the burden of disease. A structured approach enhances patient recovery and minimizes the risk of complications, particularly in vulnerable populations.