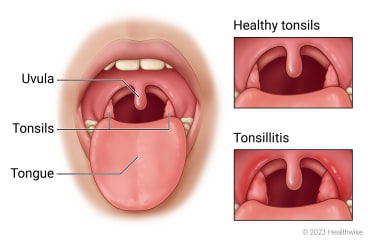
Tonsillitis is an inflammation of the tonsils, the two lymphoid tissues located at the back of the throat. It is commonly caused by viral or bacterial infections and is especially prevalent among children, though adults may also be affected. While most cases are self-limiting, recurrent or severe episodes may require medical or surgical intervention.
Key Symptoms of Tonsillitis: Recognizing the Signs
Patients with tonsillitis typically present with a range of symptoms that vary based on the causative agent and severity. Prompt recognition is essential for effective treatment.
Common Symptoms Include:
- Sore throat and difficulty swallowing
- Swollen, red tonsils, sometimes with white or yellow coating
- Fever and chills
- Swollen lymph nodes in the neck
- Headache and fatigue
- Hoarseness or loss of voice
- Bad breath (halitosis)
In children, additional symptoms may include nausea, abdominal pain, and drooling due to difficulty swallowing.
Causes of Tonsillitis: Viral and Bacterial Origins
Tonsillitis is primarily caused by infectious pathogens, with viruses accounting for the majority of cases.
Viral Causes
- Adenovirus
- Rhinovirus
- Influenza virus
- Epstein-Barr virus (EBV) — associated with mononucleosis
- Coronavirus
Bacterial Causes
- Group A Streptococcus (GAS) — the most common bacterial agent
- Other streptococcal groups
- Mycoplasma pneumoniae
- Chlamydia pneumoniae
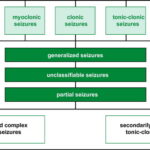
Types of Tonsillitis: Acute, Chronic, and Recurrent
Tonsillitis is classified into different types based on the duration and frequency of episodes.
Acute Tonsillitis
- Sudden onset
- Usually resolves within 7–10 days
- Most cases are viral
Chronic Tonsillitis
- Persistent inflammation lasting more than 3 months
- May be associated with tonsil stones (tonsilloliths) and halitosis
Recurrent Tonsillitis
- Multiple episodes within a year (e.g., >7 in one year or >3 annually over 3 years)
- Often a consideration for tonsillectomy
Diagnosis of Tonsillitis: Clinical and Laboratory Evaluation
Diagnosis begins with a physical examination, followed by targeted investigations:
Clinical Examination
- Inspection of the throat for redness, swelling, exudates
- Palpation of cervical lymph nodes
Diagnostic Tests
- Throat swab and culture to detect Streptococcus pyogenes
- Rapid antigen detection test (RADT) for strep throat
- Monospot test if Epstein-Barr virus is suspected
- Complete blood count (CBC) to differentiate between viral and bacterial causes
Tonsillitis Treatment: Medical, Supportive, and Surgical Options
Treatment varies based on etiology, symptom severity, and recurrence.
1. Symptomatic and Supportive Treatment
- Hydration and rest
- Warm saline gargles
- Analgesics and antipyretics such as ibuprofen or acetaminophen
- Throat lozenges and humidifiers to ease discomfort
2. Antibiotic Therapy
Prescribed when a bacterial infection is confirmed or strongly suspected.
| Antibiotic | Duration | Notes |
|---|---|---|
| Penicillin V | 10 days | First-line for strep throat |
| Amoxicillin | 10 days | Common alternative |
| Azithromycin | 5 days | For penicillin-allergic individuals |
| Clindamycin | 10 days | For resistant or recurrent infections |
3. Surgical Intervention: Tonsillectomy
Indicated in cases of:
- Recurrent or chronic tonsillitis
- Obstructive sleep apnea due to enlarged tonsils
- Peritonsillar abscess (quinsy)
- Difficulty breathing or swallowing
Tonsillitis in Children vs. Adults: A Comparative Perspective
While tonsillitis affects both age groups, clinical approach and implications may vary.
Children
- More likely to develop recurrent infections
- Tonsillectomy is more commonly performed
- Rapid streptococcal testing is more frequently utilized
Adults
- Often linked to EBV or chronic infection
- Greater risk of complications such as abscess
- Conservative management preferred initially
Potential Complications of Untreated Tonsillitis
If left unmanaged, especially bacterial tonsillitis, the following complications may arise:
- Peritonsillar abscess — requires drainage
- Rheumatic fever
- Post-streptococcal glomerulonephritis
- Otitis media
- Obstructive sleep apnea
- Sepsis in immunocompromised individuals
Preventive Measures for Tonsillitis
Preventing tonsillitis involves both lifestyle modifications and infection control practices:
- Regular handwashing
- Avoiding contact with infected individuals
- Refraining from sharing utensils or cups
- Maintaining a healthy immune system through nutrition and rest
- Proper treatment of strep throat to prevent recurrence
Recovery Timeline and Home Care Tips
Typical Recovery Time
- Viral tonsillitis: 5–7 days with rest and fluids
- Bacterial tonsillitis: Improvement within 48 hours of antibiotics
Home Care Recommendations
- Warm teas and broths
- Cold foods (e.g., ice cream) to reduce inflammation
- Pain relief sprays
- Avoid smoking and irritants
- Complete entire course of antibiotics
Frequently Asked Questions:
What is the fastest way to treat tonsillitis?
Prompt use of antibiotics for bacterial cases, combined with rest, fluids, and analgesics, often speeds up recovery.
Can tonsillitis go away on its own?
Yes, viral tonsillitis typically resolves without antibiotics, but bacterial cases require treatment to avoid complications.
How contagious is tonsillitis?
Tonsillitis caused by bacteria or viruses is highly contagious, especially in the first few days of symptom onset.
When should I see a doctor for tonsillitis?
Seek medical attention if symptoms last longer than 3 days, if there is difficulty breathing, or if high fever persists.
Is tonsillectomy necessary?
Tonsillectomy is considered when tonsillitis is recurrent, severe, or causes airway obstruction or complications.
Strategic Management of Tonsillitis for Optimal Health
Tonsillitis is a common yet potentially serious condition that necessitates a tailored approach based on the underlying cause. Through accurate diagnosis, prompt treatment, and preventive care, both acute and chronic forms can be managed effectively. In recurrent or complicated cases, surgical intervention remains a viable and often curative option. Educating patients and implementing early intervention strategies are vital to reducing disease burden and improving long-term outcomes.