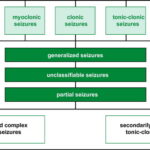
Tonic-clonic epilepsy, formerly referred to as grand mal epilepsy, is a type of generalized seizure disorder characterized by sudden loss of consciousness, violent muscle contractions, and convulsions. These seizures affect both hemispheres of the brain simultaneously and are considered one of the most recognizable forms of epilepsy. The condition can occur at any age and may be idiopathic or secondary to an underlying neurological or systemic disorder.
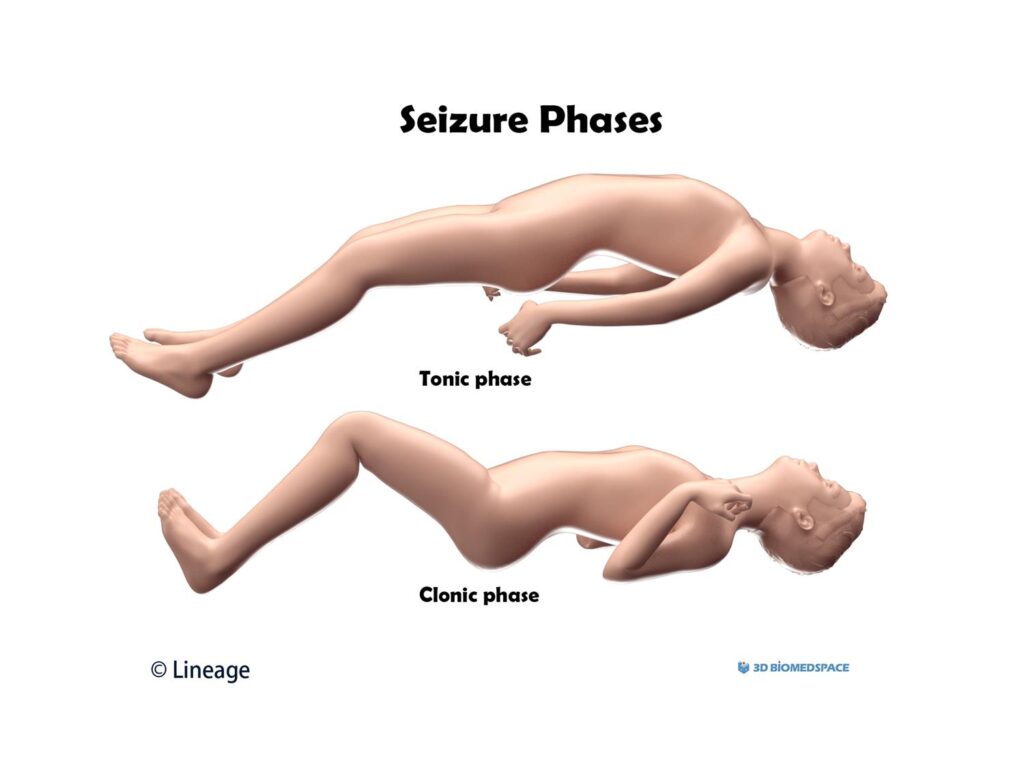
Phases of a Tonic-Clonic Seizure
A tonic-clonic seizure occurs in two distinct phases:
- Tonic Phase: This phase involves sustained muscle stiffening lasting 10–20 seconds. The person typically loses consciousness and may fall if standing. The airway muscles tighten, causing a characteristic cry or groan.
- Clonic Phase: Following the tonic contraction, rhythmic jerking movements of the limbs begin. This phase may last 30–60 seconds and often results in cyanosis, tongue biting, and urinary incontinence.
Postictal State
After the seizure ends, the individual enters a postictal state marked by confusion, headache, drowsiness, or even temporary amnesia.
Causes and Risk Factors of Generalized Tonic-Clonic Seizures
Primary Causes
- Genetic Epilepsy Syndromes
- Idiopathic Generalized Epilepsy
- Structural Brain Abnormalities
- Neurodevelopmental Disorders
Secondary (Symptomatic) Causes
- Head trauma
- Brain tumors
- Cerebral infections (e.g., meningitis, encephalitis)
- Stroke
- Metabolic imbalances (hypoglycemia, hyponatremia)
- Alcohol or drug withdrawal
Triggers
- Sleep deprivation
- Flashing lights (photosensitive epilepsy)
- Emotional stress
- Hormonal fluctuations
- Non-compliance with medication
Recognizing the Symptoms of Tonic-Clonic Epilepsy
Pre-Ictal (Aura) Symptoms
While not always present, some patients experience a prodrome or aura, which may include:
- Visual disturbances
- Auditory hallucinations
- Nausea
- Déjà vu sensation
- Rising epigastric discomfort
Ictal Symptoms
- Sudden collapse or fall
- Loud cry or groan
- Rigidity followed by jerking movements
- Cyanosis (bluish lips or skin)
- Foaming at the mouth
- Involuntary urination or defecation
Postictal Symptoms
- Confusion
- Disorientation
- Muscle soreness
- Headache
- Deep sleep
Diagnostic Evaluation for Tonic-Clonic Epilepsy
Accurate diagnosis requires clinical assessment, neurological examination, and diagnostic imaging.
Electroencephalogram (EEG)
- Primary tool to detect abnormal electrical activity
- Generalized spike-and-wave discharges often seen
Neuroimaging
- MRI (Magnetic Resonance Imaging): Detects structural brain lesions
- CT scan: Used in emergency settings to exclude acute causes
Laboratory Investigations
- Blood glucose, electrolytes, renal and liver function
- Toxicology screening (in suspected drug-induced seizures)
- Lumbar puncture if infection is suspected
Differential Diagnosis
- Syncope
- Psychogenic non-epileptic seizures
- Cardiac arrhythmias
- Movement disorders
Treatment Options for Tonic-Clonic Epilepsy
Acute Management
During a seizure:
- Ensure the person is in a safe environment
- Turn the person on their side to prevent aspiration
- Do not restrain or place objects in the mouth
- Monitor duration; seek emergency help if it lasts >5 minutes (status epilepticus)
Long-Term Pharmacologic Treatment
First-Line Antiepileptic Drugs (AEDs):
| Medication | Mechanism | Typical Dose Range | Notes |
|---|---|---|---|
| Valproic Acid | Increases GABA availability | 10–60 mg/kg/day | Broad-spectrum, teratogenic |
| Levetiracetam | Binds synaptic vesicle protein SV2A | 500–3000 mg/day | Fewer drug interactions |
| Lamotrigine | Inhibits voltage-sensitive sodium channels | 100–500 mg/day | Slow titration needed due to rash risk |
| Topiramate | Enhances GABA, inhibits glutamate | 100–400 mg/day | May cause cognitive side effects |
| Phenytoin | Sodium channel blocker | 300–600 mg/day | Narrow therapeutic index |
Non-Pharmacological Interventions
- Ketogenic diet: High-fat, low-carb diet proven effective in drug-resistant cases
- Vagus Nerve Stimulation (VNS): Implanted device reduces seizure frequency
- Responsive Neurostimulation (RNS): Delivers targeted electrical stimulation
- Surgical options: Reserved for patients with focal onset progressing to generalized seizures
Prognosis and Quality of Life Considerations
With appropriate treatment, many individuals achieve full seizure control or significant reduction in frequency. However, prognosis depends on:
- Underlying cause
- Response to medication
- Medication adherence
- Presence of comorbid conditions
Psychosocial Impact
- Driving restrictions
- Employment limitations
- Social stigma
- Mental health challenges (anxiety, depression)
Supportive counseling, patient education, and lifestyle adjustments are essential components of comprehensive care.
Preventive Strategies and Safety Measures
- Maintain strict adherence to medication
- Avoid known triggers
- Get adequate sleep
- Use medical ID bracelets
- Educate family and peers on first aid for seizures
Frequently Asked Questions:
What causes tonic-clonic epilepsy?
It can result from genetic syndromes, brain injuries, tumors, infections, metabolic issues, or unknown (idiopathic) origins.
Can tonic-clonic epilepsy be cured?
While not always curable, many individuals achieve long-term seizure control with medication and lifestyle management.
Is tonic-clonic epilepsy dangerous?
Seizures can lead to falls, injuries, and rarely, sudden unexpected death in epilepsy (SUDEP), especially in uncontrolled cases.
How is tonic-clonic epilepsy different from focal epilepsy?
Tonic-clonic seizures involve both brain hemispheres from onset, while focal seizures begin in a specific region.
What should I do if someone has a tonic-clonic seizure?
Ensure safety, roll them onto their side, time the seizure, and seek help if it exceeds five minutes.
Managing Tonic-Clonic Epilepsy Effectively
Tonic-clonic epilepsy is a serious yet manageable neurological condition. Timely diagnosis, evidence-based treatment, lifestyle adaptation, and ongoing support systems are crucial in enhancing quality of life and minimizing seizure burden. A comprehensive, individualized approach ensures optimal outcomes and long-term well-being.