Tinea versicolor, also known as pityriasis versicolor, is a chronic superficial fungal infection of the skin caused by the Malassezia species—a lipophilic yeast that is part of the normal skin flora. This condition leads to discolored patches on the skin, often resulting in cosmetic concerns, especially in individuals with darker skin tones or during warmer months when the lesions become more apparent.

Etiology: What Causes Tinea Versicolor?
The primary causative organism is Malassezia furfur, among other Malassezia species, which thrive in seborrheic (oil-rich) areas of the body. These yeasts can shift from a harmless commensal phase to a pathogenic one under certain triggers:
- Hot and humid climates
- Excessive sweating
- Oily skin types
- Weakened immune response
- Hormonal changes, especially during adolescence
- Use of oily cosmetics or lotions
The yeast transforms into its mycelial form, which induces skin inflammation and disrupts melanocyte function, leading to hypopigmented or hyperpigmented macules.
Risk Factors for Tinea Versicolor Development
While tinea versicolor can affect anyone, specific factors increase susceptibility:
- Adolescents and young adults (peak sebaceous activity)
- Residents of tropical or subtropical climates
- Immunocompromised patients
- Individuals using systemic corticosteroids
- Excessive use of greasy skincare products
- Athletes and gym users exposed to prolonged sweating
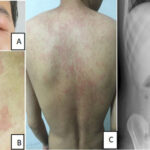
Clinical Presentation: Signs and Symptoms of Tinea Versicolor
Key Characteristics:
- Flat, oval or round macules or patches
- Color variations: hypopigmented (light), hyperpigmented (dark), pink, or tan
- Fine scaling on affected skin, especially noticeable on stretching or scraping (evoked scale sign)
- Commonly seen on:
- Upper trunk
- Neck
- Upper arms
- Occasionally on the face or abdomen
Symptoms:
- Usually asymptomatic
- Occasionally, mild itching, especially with heat or sweating
- Cosmetic distress due to discoloration
Differential Diagnosis: Conditions That Mimic Tinea Versicolor
Accurate diagnosis requires differentiation from other skin disorders with similar appearance:
- Vitiligo – Total depigmentation with no scaling
- Pityriasis alba – Hypopigmented patches in children, mild scaling
- Seborrheic dermatitis – Greasy scales on scalp, eyebrows, nasolabial folds
- Post-inflammatory hypopigmentation
- Erythrasma – Bacterial infection, coral-red fluorescence under Wood’s lamp
Diagnostic Techniques for Confirming Tinea Versicolor
Clinical Examination
- Visible pattern of discoloration and fine scaling
- Distribution in seborrheic areas
Wood’s Lamp Examination
- Affected areas fluoresce yellow-green under ultraviolet light due to presence of Malassezia
KOH Preparation (Potassium Hydroxide Test)
- Scraped skin samples examined microscopically
- Presence of “spaghetti and meatballs” appearance (hyphae and spores)
Dermoscopy
- Reveals fine scaling and pigment alteration around hair follicles
Treatment Modalities for Tinea Versicolor
Effective treatment requires elimination of active infection and prevention of recurrence.
Topical Antifungal Therapy (First-Line for Mild to Moderate Cases)
Common Agents:
- Selenium sulfide 2.5% lotion or shampoo – Applied to affected areas and rinsed after 10–15 minutes
- Ketoconazole 2% shampoo or cream
- Ciclopirox olamine 1%
- Clotrimazole, Miconazole, Terbinafine creams
Application Protocol: Apply once or twice daily for 1–4 weeks based on severity and agent used.
Systemic Antifungal Therapy (For Extensive or Recurrent Cases)
Oral Medications:
- Fluconazole – 300 mg once weekly for 2–4 weeks
- Itraconazole – 200 mg daily for 5–7 days
- Ketoconazole – 400 mg single dose, with caution due to hepatic risk
Note: Systemic agents are particularly effective for resistant or widespread infections but require liver function monitoring.
Prevention and Long-Term Management
Given its recurrent nature, preventive measures are essential:
- Avoid excessive sweating and wear breathable, loose-fitting clothes
- Bathe promptly after workouts or heat exposure
- Use non-comedogenic, oil-free skincare products
- Monthly use of antifungal shampoo or body wash (e.g., ketoconazole or selenium sulfide) as maintenance
- Avoid sharing towels or clothing with infected individuals
- Maintain regular hygiene with pH-balanced cleansers
Tinea Versicolor in Special Populations
Pediatric Patients
- Often presents with hypopigmented patches on face or trunk
- Requires mild topical antifungals, often under medical supervision
Pregnancy
- Topical treatments are preferred
- Avoid systemic antifungals unless clinically warranted
Immunocompromised Patients
- Increased risk of widespread, recurrent infections
- Require aggressive and longer-duration therapy
Complications and Recurrence
Though not dangerous, tinea versicolor can lead to:
- Persistent skin discoloration, which may take weeks or months to normalize
- Psychosocial distress, especially when affecting visible areas
- Frequent relapses during hot and humid seasons
Frequently Asked Questions:
Is tinea versicolor contagious?
No. While it is caused by a fungus, tinea versicolor is not considered contagious as the organism is part of the normal skin flora.
Can tinea versicolor go away on its own?
Rarely. In some cases, especially in cooler months, lesions may regress. However, active treatment is often necessary to resolve the infection and scaling.
Does the discoloration remain after treatment?
Yes. Pigment changes may persist for several weeks even after the infection is cleared. This is due to residual melanocyte dysfunction, not treatment failure.
What is the best treatment for tinea versicolor?
For mild cases, topical antifungals such as ketoconazole or selenium sulfide are effective. For severe or recurring cases, oral antifungals may be necessary.
How can I stop tinea versicolor from coming back?
Regular use of prophylactic antifungal body wash, maintaining dry and clean skin, and avoiding excessive oil or sweat buildup help reduce recurrence.
Essential Insights on Tinea Versicolor
- Caused by Malassezia yeast, tinea versicolor leads to discolored, scaly skin patches.
- Common in hot, humid environments and among young adults.
- Diagnosed via clinical signs, Wood’s lamp, and KOH test.
- Treated effectively with topical or systemic antifungals.
- Requires ongoing maintenance and preventive care due to its tendency to recur.