Tinea pedis, commonly known as athlete’s foot, is a contagious fungal infection affecting the feet, particularly the interdigital spaces, soles, and sides. It is one of the most prevalent dermatophytoses worldwide, caused by fungi that thrive in warm, moist environments. Despite being treatable, it often recurs without proper management and hygiene.

Etiology: What Causes Tinea Pedis?
Tinea pedis is caused by keratinophilic fungi—primarily dermatophytes that feed on the keratin found in the stratum corneum of the skin. The most common causative organisms include:
- Trichophyton rubrum (most frequent)
- Trichophyton interdigitale
- Epidermophyton floccosum
These fungi are transmitted through direct skin contact or by contact with contaminated surfaces such as communal showers, locker rooms, shoes, and socks.
Risk Factors: Who Is Most Susceptible?
Certain individuals are more prone to tinea pedis due to environmental or physiological factors. These include:
- Athletes and gym-goers
- People wearing occlusive footwear for long durations
- Individuals with hyperhidrosis (excessive foot sweating)
- Diabetes patients
- Immunocompromised individuals
- Military personnel and factory workers
- Individuals sharing towels, socks, or shoes
Clinical Variants and Symptoms of Tinea Pedis
Tinea pedis manifests in four primary clinical forms, each with distinct characteristics:
1. Interdigital Type
- Most common form
- Fissuring, scaling, and maceration between the toes (especially between the 4th and 5th)
- Itching, burning sensation, and malodor
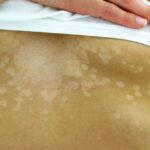
2. Moccasin Type (Chronic Hyperkeratotic)
- Involves the soles, heels, and sides of the feet
- Dry, thick, scaly skin resembling a moccasin
- Often resistant to topical treatments
3. Vesiculobullous Type
- Less common
- Vesicles or bullae filled with clear fluid, primarily on the sole or instep
- Painful, itchy eruptions that may rupture and crust
4. Ulcerative Type
- Severe form, typically in immunocompromised or diabetic patients
- Rapid ulceration, erosion, and secondary bacterial infection
Differential Diagnoses: Similar Foot Conditions to Consider
Tinea pedis must be carefully distinguished from other dermatoses:
- Eczema: Symmetrical, intensely itchy, often with vesicles
- Psoriasis: Thick, silvery scales with well-demarcated borders
- Contact dermatitis: Redness and inflammation due to allergen or irritant exposure
- Pitted keratolysis: Bacterial infection causing crater-like lesions and odor
- Palmoplantar keratoderma: Diffuse thickening of soles (hereditary or acquired)
Diagnostic Approaches for Confirming Tinea Pedis
KOH Microscopy
- Skin scrapings examined under a microscope after potassium hydroxide (KOH) preparation
- Presence of branching septate hyphae confirms dermatophyte infection
Fungal Culture
- Gold standard for precise identification
- Samples inoculated on Sabouraud dextrose agar
Dermoscopy
- Assists in visualizing specific features like white scales, dotted vessels, and vessels in the furrows
Skin Biopsy
- Rarely needed, used for chronic or atypical presentations
Treatment Strategies for Tinea Pedis
Topical Antifungal Therapy (First-Line)
Effective for mild to moderate cases, especially interdigital and moccasin types.
Commonly Used Topicals:
- Terbinafine 1% – highly fungicidal
- Clotrimazole 1%
- Econazole nitrate
- Miconazole
- Naftifine
Application Guideline: Apply twice daily for 2–4 weeks, including at least 1 inch beyond the lesion margin.
Systemic Antifungal Therapy
Recommended for extensive, resistant, or vesiculobullous forms, or when nails are also infected (onychomycosis).
Common Oral Antifungals:
- Terbinafine 250 mg once daily for 2–6 weeks
- Itraconazole 100–200 mg/day for 2–4 weeks
- Fluconazole 150 mg once weekly for 4–6 weeks
Adjunctive Therapies:
- Keratolytics (e.g., salicylic acid) to reduce scaling and enhance drug penetration
- Antiseptic soaks (e.g., potassium permanganate for vesicular form)
- Topical corticosteroids (only in inflammatory tinea under antifungal coverage)
Prevention: Best Practices to Avoid Recurrence
Proper hygiene and lifestyle modifications are essential for preventing reinfection:
- Wash and dry feet thoroughly, especially between toes
- Use antifungal foot powders in shoes and socks
- Avoid walking barefoot in communal showers or locker rooms
- Wear breathable footwear and change socks daily
- Disinfect shoes regularly using UV sanitizers or antifungal sprays
- Avoid sharing footwear, socks, or towels
- Treat coexisting fungal infections (nails, groin)
Complications of Untreated Tinea Pedis
Neglected or mismanaged infections can result in:
- Tinea incognito due to inappropriate corticosteroid use
- Secondary bacterial infections like cellulitis
- Lymphangitis or lymphadenitis
- Spread to nails (onychomycosis) and other body parts (tinea corporis)
- Recurrent, chronic infection with resistant strains
Prognosis and Follow-Up
With timely and appropriate treatment, most patients experience complete resolution. However, chronic or recurrent cases may require extended antifungal therapy, ongoing preventive care, and footwear hygiene to maintain remission.
Follow-up evaluations should assess for:
- Resolution of clinical signs
- Co-infections or misdiagnoses
- Medication adherence
- Recurrent exposure risks
Frequently Asked Questions:
Is tinea pedis contagious?
Yes, tinea pedis is highly contagious and spreads through skin contact or contaminated surfaces like locker rooms, towels, or footwear.
How long does tinea pedis take to heal?
Mild infections respond within 2 to 4 weeks of topical therapy. Severe or recurrent infections may require oral antifungals for up to 6 weeks.
Can tinea pedis spread to other parts of the body?
Yes. It can spread to nails, groin (tinea cruris), hands (tinea manuum), or trunk (tinea corporis) if not treated properly.
What is the best over-the-counter treatment?
Topical antifungals like terbinafine, clotrimazole, or miconazole are effective OTC treatments for most cases of athlete’s foot.
Is tinea pedis more common in summer?
Yes. Hot and humid conditions promote fungal growth, making tinea pedis more prevalent in the summer months and tropical regions.
Key Takeaways on Tinea Pedis
- Tinea pedis is a widespread fungal infection of the feet caused by dermatophytes.
- Clinical types include interdigital, moccasin, vesiculobullous, and ulcerative forms.
- Diagnosis is confirmed through KOH prep, culture, or dermoscopy.
- Treatment involves topical or systemic antifungals, depending on severity.
- Preventive hygiene and foot care are critical to prevent reinfection and complications.