Thyrotoxicosis crisis, also known as thyroid storm, is an acute, life-threatening condition characterized by an extreme surge in thyroid hormone activity. It represents the most severe form of thyrotoxicosis and requires immediate medical intervention. Often precipitated by stressors in patients with untreated or inadequately managed hyperthyroidism, this endocrine emergency can lead to multiorgan dysfunction and death if not promptly addressed.
Pathophysiology of Thyroid Storm
The underlying mechanism of a thyrotoxicosis crisis involves a sudden increase in the bioavailability and effect of triiodothyronine (T3) and thyroxine (T4). Although serum levels may not significantly differ from uncomplicated thyrotoxicosis, it is the tissue sensitivity, adrenergic surge, and altered metabolism that precipitate the crisis.
Common Triggers:
- Infections (e.g., pneumonia, sepsis)
- Surgery, trauma, or childbirth
- Discontinuation of antithyroid medications
- Iodine exposure (e.g., contrast media)
- Diabetic ketoacidosis
- Myocardial infarction or stroke
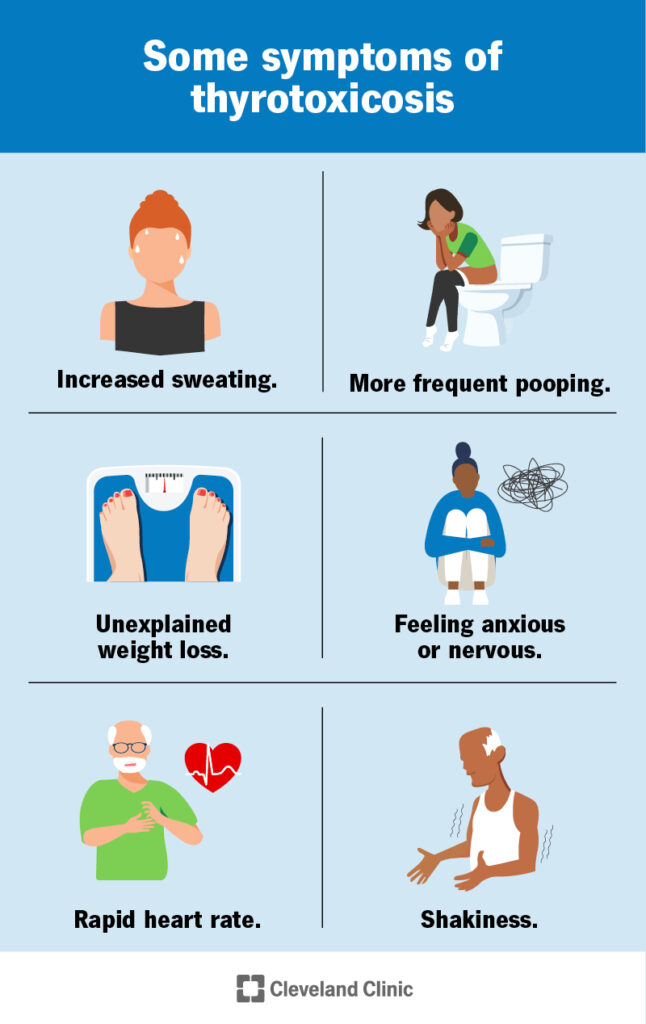
Clinical Presentation: Recognizing the Signs of Thyrotoxicosis Crisis
Patients present with a hypermetabolic state and multiple organ system involvement.
Cardinal Features:
| System | Manifestations |
|---|---|
| Central Nervous System | Agitation, delirium, psychosis, seizures, coma |
| Cardiovascular | Tachycardia, atrial fibrillation, CHF, hypotension |
| Thermoregulatory | Fever often > 104°F (40°C) |
| Gastrointestinal-Hepatic | Nausea, vomiting, diarrhea, jaundice, hepatic failure |
| Other | Tremors, dehydration, profound weakness |
Diagnostic Criteria for Thyrotoxicosis Crisis
Although no single test confirms thyroid storm, clinical scoring systems help standardize the diagnosis.
Burch-Wartofsky Point Scale (BWPS):
This scoring system is widely used to assess the likelihood of a thyrotoxic crisis.
- <25: Unlikely
- 25–44: Impending crisis
- ≥45: Highly suggestive of thyroid storm
Laboratory Findings in Thyrotoxicosis Crisis
While lab values may resemble those of uncomplicated thyrotoxicosis, certain indicators point to crisis severity:
- TSH: Suppressed (often <0.01 mIU/L)
- Free T4 and T3: Elevated
- Liver enzymes: Elevated AST/ALT, bilirubin
- Hyperglycemia and lactic acidosis
- Leukocytosis or leukopenia in infection
Differential Diagnosis
Rapid distinction from other critical conditions is essential:
- Sepsis
- Neuroleptic malignant syndrome
- Pheochromocytoma crisis
- Heat stroke
- Delirium tremens
- Malignant hyperthermia
Emergency Management and Treatment Protocols
Thyrotoxicosis crisis requires aggressive, multi-pronged therapy targeting thyroid hormone production, release, peripheral action, and underlying cause.
Stepwise Management Approach:
- Supportive Care:
- ICU monitoring
- IV fluids, oxygen, electrolyte correction
- Cooling blankets and antipyretics (avoid aspirin)
- Adrenergic Blockade:
- Propranolol 60–80 mg PO q6h or IV 1–2 mg q15min as needed
- Alternative: Esmolol for precise titration
- Inhibition of Hormone Synthesis:
- Propylthiouracil (PTU): 500–1000 mg loading dose, then 250 mg q4h
- Preferred in thyroid storm due to peripheral T4 to T3 inhibition
- Methimazole: Alternative when PTU not tolerated
- Propylthiouracil (PTU): 500–1000 mg loading dose, then 250 mg q4h
- Blockade of Hormone Release:
- Iodine (Lugol’s or SSKI): Given ≥1 hour after PTU, 5 drops PO q6h
- Inhibition of Peripheral Conversion:
- Hydrocortisone 100 mg IV q8h or dexamethasone 2 mg IV q6h
- Also helps manage relative adrenal insufficiency
- Treatment of Precipitating Factors:
- Empiric broad-spectrum antibiotics for sepsis
- Control of arrhythmias, DKA, or other comorbidities
- Advanced Measures:
- Plasmapheresis or cholestyramine to remove circulating hormones
- Therapeutic plasma exchange (TPE) in refractory cases
Prognosis and Outcomes
Prompt treatment significantly improves survival. Untreated, the mortality rate exceeds 80%; with intensive care, it falls to approximately 10–30%.
Poor Prognostic Indicators:
- Delay in diagnosis or treatment
- Cardiac arrhythmias
- Hepatic failure
- Advanced age
- Multiorgan dysfunction
Long-Term Management and Follow-Up
Post-crisis stabilization involves transitioning to long-term antithyroid therapy, radioactive iodine ablation, or thyroidectomy, depending on the underlying cause.
Monitoring Includes:
- Regular thyroid function tests
- Adjustment of beta-blockers
- Surveillance for hypothyroidism
- Continued treatment of precipitating illness
Frequently Asked Questions:
What distinguishes thyrotoxicosis crisis from regular hyperthyroidism?
A thyrotoxicosis crisis presents with systemic decompensation, such as high fever, altered mental status, and cardiac instability, unlike stable hyperthyroidism.
Is thyroid storm a medical emergency?
Yes, it is a critical emergency with rapid deterioration and high mortality without intensive care.
Can thyroid storm recur?
Yes, especially if the underlying thyroid disorder remains untreated or if another precipitating factor arises.
How quickly does treatment work?
Clinical improvement is usually observed within 24–72 hours with aggressive, appropriate management.
Are there permanent effects from a thyrotoxicosis crisis?
If treated promptly, patients may recover fully, though cardiac or hepatic complications can result in lasting effects.
Thyrotoxicosis crisis, or thyroid storm, demands swift recognition and urgent intervention. Through a structured approach involving beta-blockade, thionamides, iodine administration, corticosteroids, and correction of triggers, we can significantly reduce morbidity and mortality. Continuous monitoring and transition to definitive therapy are essential to prevent recurrence and ensure long-term stabilization.