Thyrotoxicosis is a clinical state resulting from elevated levels of circulating thyroid hormones—thyroxine (T4) and triiodothyronine (T3)—regardless of their source. Unlike hyperthyroidism, which implies increased synthesis of thyroid hormones, thyrotoxicosis encompasses both endogenous overproduction and exogenous sources, including medication overuse and thyroiditis.
Classification of Thyrotoxicosis by Etiology
Thyrotoxicosis is classified based on the origin of hormone excess, which can be due to increased synthesis, release, or external administration.
Common Causes of Thyrotoxicosis
Graves’ Disease
- Autoimmune disorder causing continuous stimulation of the TSH receptor
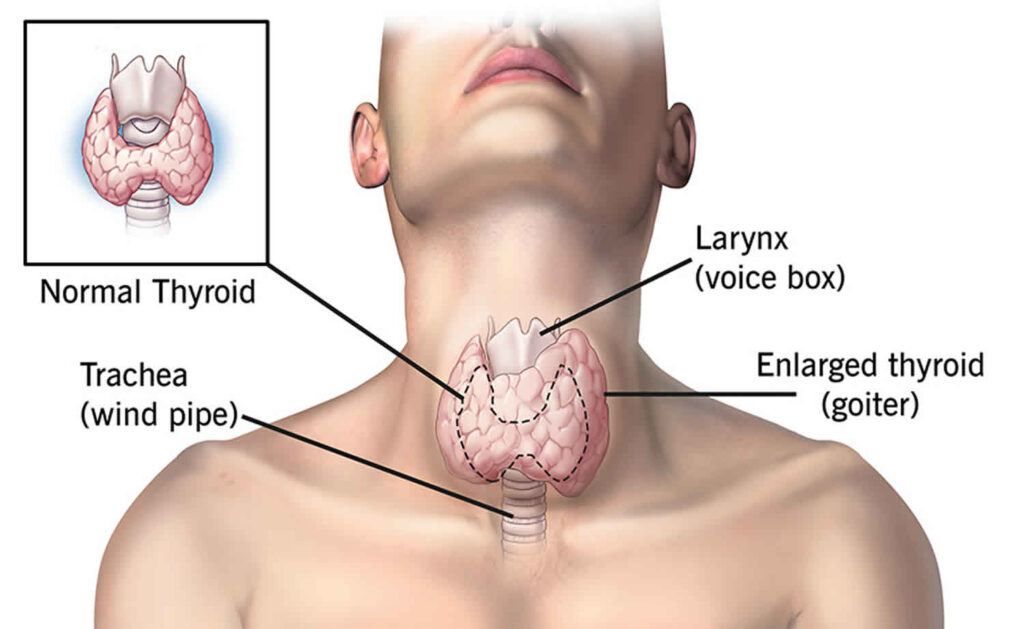
- Symptoms: Goiter, ophthalmopathy (exophthalmos), pretibial myxedema
- Labs: Suppressed TSH, elevated free T4/T3, positive TSI (thyroid-stimulating immunoglobulins)
Toxic Multinodular Goiter (Plummer’s Disease)
- Nodular enlargement of the thyroid leading to autonomous hormone production
- Seen in older adults, often with long-standing goiter
- Absence of eye signs
Toxic Adenoma
- Solitary, functional nodule autonomously producing thyroid hormones
- Detected via thyroid scan showing “hot” nodule with suppressed background
Subacute and Silent Thyroiditis
- Transient thyrotoxicosis from hormone leakage due to glandular inflammation
- Subacute (painful) often post-viral; Silent (painless) often autoimmune
Exogenous Thyroid Hormone Intake (Factitious Thyrotoxicosis)
- Intentional or accidental ingestion of levothyroxine
- Suppressed TSH, elevated T4, low thyroglobulin
Struma Ovarii and TSH-Secreting Tumors
- Rare causes involving ectopic thyroid tissue or pituitary adenomas
- TSH-producing tumors show elevated TSH despite high T3/T4
Clinical Features and Symptoms of Thyrotoxicosis
The excess thyroid hormone exerts multisystem effects:
| System | Clinical Manifestations |
|---|---|
| General | Weight loss, fatigue, heat intolerance |
| Cardiovascular | Palpitations, tachycardia, atrial fibrillation |
| Neuromuscular | Tremors, hyperreflexia, muscle weakness |
| Gastrointestinal | Increased appetite, diarrhea |
| Reproductive | Menstrual irregularities, infertility |
| Dermatologic | Warm moist skin, hair thinning |
| Ophthalmic | Lid lag, proptosis (in Graves’) |
| Psychiatric | Anxiety, irritability, insomnia |
Thyroid Storm: The Life-Threatening Extreme
Thyroid storm is a medical emergency representing severe, acute thyrotoxicosis. It is often precipitated by infection, surgery, trauma, or withdrawal of antithyroid drugs.
Features:
- Hyperpyrexia (>104°F)
- Severe tachycardia or arrhythmias
- Agitation, delirium
- Heart failure, hypotension
- Gastrointestinal disturbances (vomiting, diarrhea)
Management: Requires ICU admission, beta-blockers, thionamides, iodine, corticosteroids, and supportive care.
Diagnostic Evaluation of Thyrotoxicosis
Thyroid Function Tests
- TSH: Suppressed in most cases
- Free T4 and T3: Elevated; T3 toxicosis is not uncommon
- T3/T4 Ratio: Elevated in Graves’ and toxic adenoma
Antibody Testing
- TSI (Thyroid-Stimulating Immunoglobulin): Elevated in Graves’
- Anti-TPO and Anti-Tg Antibodies: Seen in autoimmune thyroiditis
Imaging and Functional Tests
- Radioactive Iodine Uptake (RAIU):
- Diffuse high uptake: Graves’ disease
- Focal high uptake: Toxic adenoma
- Low uptake: Thyroiditis or factitious thyrotoxicosis
- Thyroid Ultrasound:
- Detects nodules, vascularity
- Differentiates cystic from solid lesions
Management of Thyrotoxicosis: Tailored Treatment by Cause
1. Graves’ Disease
- Beta-blockers (e.g., propranolol): For symptom relief
- Antithyroid drugs: Methimazole or propylthiouracil (PTU)
- Radioactive iodine ablation: First-line in adults
- Surgery: For large goiters, eye disease, or intolerance to other treatments
2. Toxic Adenoma and Multinodular Goiter
- Radioiodine therapy: Curative
- Surgical resection: Preferred in compressive symptoms or malignancy suspicion
3. Thyroiditis
- Supportive treatment only
- NSAIDs or steroids for subacute thyroiditis
- Beta-blockers for symptomatic control
- Antithyroid drugs are not effective
4. Exogenous Thyrotoxicosis
- Discontinuation of thyroid hormone
- Beta-blockers for transient symptom management
5. TSH-Secreting Tumors and Struma Ovarii
- Surgical resection of tumor
- Somatostatin analogs may reduce TSH levels preoperatively
Monitoring and Long-Term Follow-Up
Periodic Assessment:
- TSH and free T4 levels
- Liver function and CBC (if on thionamides)
- Thyroid ultrasound in nodular disease
Risk of Recurrence:
- Graves’: ~50% relapse after stopping antithyroid drugs
- Toxic nodules: Rarely resolve without ablation or surgery
Hypothyroidism Risk:
- Common after radioactive iodine or thyroid surgery
- Requires lifelong levothyroxine replacement
Frequently Asked Questions:
What is the difference between thyrotoxicosis and hyperthyroidism?
Hyperthyroidism refers to increased thyroid hormone production, whereas thyrotoxicosis refers to elevated hormone levels, regardless of the source.
Is thyrotoxicosis curable?
Yes, most causes are treatable or manageable, with options ranging from medications to surgery and radioactive iodine.
Can thyrotoxicosis cause heart problems?
Yes, untreated thyrotoxicosis can lead to arrhythmias, especially atrial fibrillation, and heart failure in severe cases.
How is thyrotoxicosis diagnosed?
Diagnosis is based on suppressed TSH, elevated T4/T3, antibody profiles, and RAIU scans to identify the underlying cause.
Is radioactive iodine safe?
Yes, it is a widely used, safe, and effective treatment for Graves’ disease and toxic nodules, though it can lead to hypothyroidism.
Thyrotoxicosis is a multifaceted endocrine disorder with wide-ranging systemic effects and diverse etiologies. Accurate diagnosis and targeted treatment based on the underlying cause are essential for optimal patient outcomes. Through a combination of clinical assessment, laboratory testing, and imaging, we can ensure precise evaluation and effective long-term management of this condition.