Thyroiditis refers to the inflammation of the thyroid gland, a butterfly-shaped endocrine organ located in the front of the neck. This condition encompasses a spectrum of disorders characterized by various causes, clinical manifestations, and outcomes. While some forms of thyroiditis resolve spontaneously, others may progress to chronic thyroid dysfunction, requiring long-term management.
Classification of Thyroiditis: Types and Their Characteristics
Thyroiditis is categorized into several types based on the underlying cause, duration, and pathology. Each type has distinct clinical features, diagnostic requirements, and therapeutic strategies.
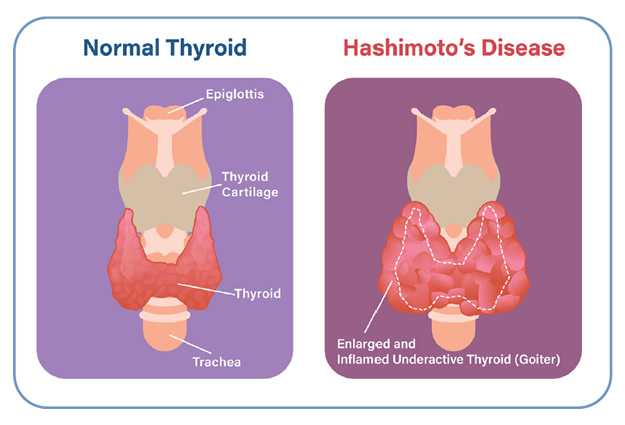
1. Hashimoto’s Thyroiditis (Chronic Lymphocytic Thyroiditis)
- Etiology: Autoimmune; T-cell mediated destruction of thyroid cells
- Demographics: More common in women aged 30–50
- Clinical Features: Fatigue, weight gain, cold intolerance, goiter
- Progression: Leads to hypothyroidism
- Markers: Elevated TSH, low T4, positive anti-TPO and anti-Tg antibodies
2. Subacute Thyroiditis (de Quervain’s Thyroiditis)
- Etiology: Post-viral inflammatory response
- Symptoms: Painful, tender thyroid gland, fever, malaise
- Phases: Hyperthyroid → Euthyroid → Hypothyroid → Recovery
- Lab Findings: Elevated ESR, low TSH (initially), high T4, low radioactive iodine uptake (RAIU)
3. Silent Thyroiditis (Painless Thyroiditis)
- Etiology: Autoimmune, often associated with other autoimmune disorders
- Presentation: Transient hyperthyroidism without pain, followed by hypothyroidism
- Often overlaps with postpartum thyroiditis
4. Acute (Suppurative) Thyroiditis
- Etiology: Bacterial infection, rare but potentially serious
- Clinical Signs: High fever, erythema, fluctuant neck mass, dysphagia
- Management: Antibiotics, surgical drainage if abscess forms
5. Postpartum Thyroiditis
- Onset: Within 12 months after delivery
- Progression: Hyperthyroid phase followed by hypothyroid phase
- Prognosis: Many return to normal thyroid function, though some develop permanent hypothyroidism
6. Drug-Induced Thyroiditis
- Common Culprits: Amiodarone, interferon-alpha, lithium
- Mechanism: Direct toxic or immune-modulating effects
- Diagnosis: Clinical history and ruling out other causes
Clinical Presentation: Recognizing Thyroiditis Symptoms
Symptoms vary depending on the type and phase of thyroiditis:
| Phase/Type | Common Symptoms |
|---|---|
| Hyperthyroid (early) | Anxiety, tremors, palpitations, weight loss |
| Hypothyroid (late/chronic) | Fatigue, cold intolerance, constipation, dry skin |
| Painful types (subacute) | Neck pain radiating to jaw or ears |
| Silent types | No pain, detected incidentally or post-delivery |
Causes and Risk Factors Associated with Thyroiditis
Thyroiditis may result from autoimmune dysfunction, infections, medications, or mechanical trauma. Genetic predisposition and environmental factors also play roles.
Common Causes:
- Autoimmune dysfunction (Hashimoto’s, Silent, Postpartum)
- Viral infections (Subacute)
- Bacterial invasion (Acute suppurative)
- Drug effects (Amiodarone, lithium)
- Radiation exposure or surgery
Risk Factors:
- Female gender
- Personal or family history of autoimmune disease
- Recent pregnancy
- Viral illness
- Iodine intake abnormalities
Diagnostic Approach to Thyroiditis
A combination of laboratory tests, imaging studies, and clinical examination is used to confirm the diagnosis and guide treatment.
Key Laboratory Tests:
- TSH, Free T4, Free T3: Assess thyroid function
- Anti-TPO, Anti-Tg Antibodies: Confirm autoimmune etiology
- ESR and CRP: Indicate inflammation in subacute cases
- Thyroglobulin: Elevated in inflammatory destruction
Imaging:
- Thyroid Ultrasound: Shows heterogeneous echotexture in chronic thyroiditis
- Radioactive Iodine Uptake (RAIU):
- Low in subacute, silent, and postpartum thyroiditis
- Normal or high in Graves’ disease (differentiates causes of thyrotoxicosis)
Treatment Options for Different Types of Thyroiditis
Treatment varies significantly depending on the type, severity, and phase of the disease.
Hashimoto’s Thyroiditis:
- Lifelong levothyroxine replacement
- Regular TSH monitoring
- Goiter management if large or compressive
Subacute Thyroiditis:
- NSAIDs or corticosteroids for pain and inflammation
- Beta-blockers for symptom control in hyperthyroid phase
- No antithyroid drugs as etiology is inflammatory, not overproduction
Silent and Postpartum Thyroiditis:
- Supportive care
- Beta-blockers for hyperthyroid symptoms
- Levothyroxine in hypothyroid phase if symptomatic or TSH >10 mIU/L
Acute Suppurative Thyroiditis:
- Broad-spectrum antibiotics
- Surgical drainage for abscess formation
- Hospital admission due to potential for sepsis
Drug-Induced Thyroiditis:
- Discontinuation of offending medication
- Symptomatic management during thyroid dysfunction phases
Prognosis and Long-Term Management
The course and prognosis depend on the underlying type of thyroiditis.
- Hashimoto’s: Chronic, irreversible, requires lifelong monitoring and treatment
- Subacute: Self-limited in most cases, complete recovery in 90% of patients
- Silent/Postpartum: 20–30% progress to permanent hypothyroidism
- Acute: Excellent prognosis with prompt antibiotic therapy
Long-Term Follow-Up:
- TSH testing every 6–12 months
- Antibody levels do not correlate with disease activity
- Ultrasound monitoring in presence of nodules or goiter
Frequently Asked Questions:
What is the most common form of thyroiditis?
Hashimoto’s thyroiditis is the most prevalent, especially in women.
Is thyroiditis the same as hypothyroidism?
No. Thyroiditis is an inflammatory condition that can lead to hypothyroidism, but they are not synonymous.
Can thyroiditis be cured?
Some forms, such as subacute and silent thyroiditis, resolve on their own. Others, like Hashimoto’s, are chronic and managed rather than cured.
Is thyroiditis painful?
Only some types, like subacute and acute thyroiditis, are associated with neck pain.
Can thyroiditis cause permanent thyroid damage?
Yes. Autoimmune thyroiditis often leads to irreversible hypothyroidism over time.
Thyroiditis encompasses a diverse group of inflammatory thyroid disorders, each with unique etiologies, clinical courses, and therapeutic strategies. Accurate diagnosis based on symptoms, laboratory results, and imaging ensures appropriate and timely intervention. With vigilant monitoring and personalized care, patients can manage symptoms effectively and maintain long-term thyroid health.