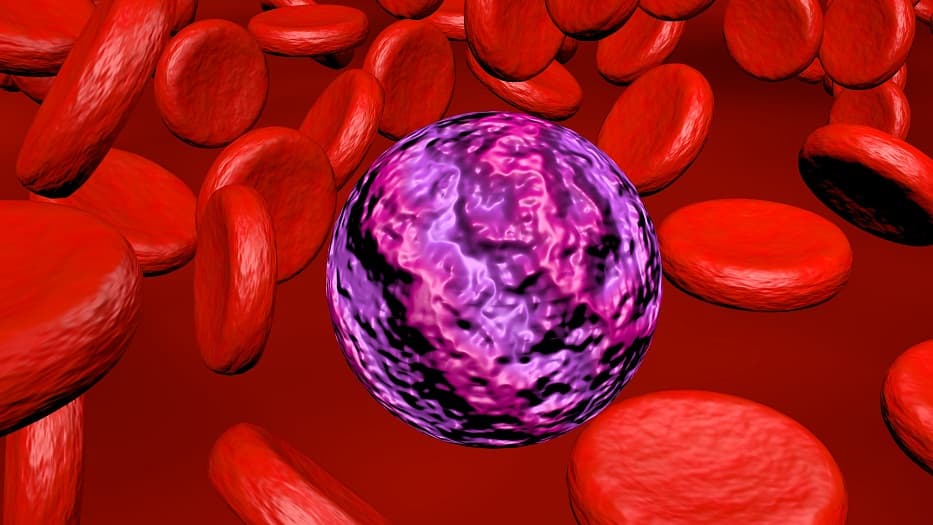
Acute myeloid leukemia (AML) is a heterogeneous hematologic malignancy characterized by clonal proliferation of myeloid precursors. Among the various subtypes, CD33-positive AML represents a critical subset with distinct diagnostic, prognostic, and therapeutic considerations. This article delves into the essential aspects of CD33-positive AML, including its pathophysiology, clinical manifestations, diagnostic criteria, and evolving treatment paradigms.
Pathophysiology of cd33 positive acute myeloid leukemia
CD33 is a sialic acid-binding immunoglobulin-like lectin expressed on the surface of myeloid progenitor cells. Its role in AML involves:
- Cellular Marker: CD33 expression is seen in approximately 85% of AML cases, making it a key target for diagnosis and therapy.
- Leukemogenesis: Aberrant signaling via CD33 promotes survival, proliferation, and resistance in leukemic cells.
- Therapeutic Target: CD33’s restricted expression on malignant cells presents opportunities for selective targeting with monoclonal antibodies and antibody-drug conjugates.
Clinical Presentation of CD33-Positive AML
The clinical manifestations of CD33-positive AML are similar to other AML subtypes and may include:
- Symptoms of Bone Marrow Failure:
- Fatigue, weakness, and pallor due to anemia
- Increased susceptibility to infections from leukopenia
- Easy bruising or bleeding caused by thrombocytopenia
- Systemic Symptoms: Fever, night sweats, and weight loss.
- Organ Involvement: Hepatosplenomegaly, lymphadenopathy, and infiltration of skin or gums.
Diagnostic Criteria and Methods
Accurate diagnosis is vital for effective treatment planning. The diagnostic approach includes:
Peripheral Blood and Bone Marrow Examination
- Complete Blood Count (CBC): Presence of blasts and abnormal cell counts.
- Bone Marrow Biopsy: Hypercellularity with increased myeloblasts (>20%).
Immunophenotyping
Flow cytometry is crucial for detecting CD33 expression, alongside other markers like CD13, CD34, and HLA-DR.
Cytogenetic and Molecular Analysis
- Chromosomal Abnormalities: Common aberrations include t(8;21), inv(16), and complex karyotypes.
- Molecular Mutations: FLT3-ITD, NPM1, and CEBPA mutations provide additional prognostic information.
Imaging
Imaging studies may be performed to assess extramedullary involvement.
Treatment Strategies for CD33-Positive AML
The treatment of CD33-positive AML integrates conventional therapies and targeted approaches:
Induction Therapy
- Cytarabine and Anthracycline-Based Regimens:
- Standard “7+3” protocol.
- Gemtuzumab Ozogamicin (GO):
- A CD33-targeted antibody-drug conjugate.
- Often incorporated in combination with chemotherapy for newly diagnosed patients.
Consolidation Therapy
- High-Dose Cytarabine (HiDAC): Preferred for patients achieving remission.
- Allogeneic Hematopoietic Stem Cell Transplantation (HSCT):
- Recommended for patients with high-risk disease or relapse.
Targeted Therapies and Experimental Approaches
- FLT3 Inhibitors: Midostaurin for FLT3-mutated AML.
- Immune-Based Strategies:
- Bispecific T-cell engagers (BiTEs) targeting CD33.
- Chimeric antigen receptor (CAR) T-cell therapies under investigation.
- Clinical Trials: Novel agents and combinations for refractory cases.
Prognosis and Survival Outcomes
Prognosis in CD33-positive AML depends on multiple factors:
- Age and Performance Status: Older patients tend to have worse outcomes.
- Cytogenetics and Molecular Profile: Favorable, intermediate, or adverse risk groups based on specific aberrations.
- Treatment Response: Minimal residual disease (MRD) negativity correlates with improved survival.
Survival Rates
- Overall survival varies widely, with younger patients achieving higher remission rates compared to older adults.
CD33-positive AML represents a distinct and clinically significant subset of AML. Advances in molecular diagnostics and targeted therapies, such as gemtuzumab ozogamicin and emerging immunotherapies, have transformed the management landscape. Continued research and clinical trials hold promise for further improving outcomes in this challenging malignancy.