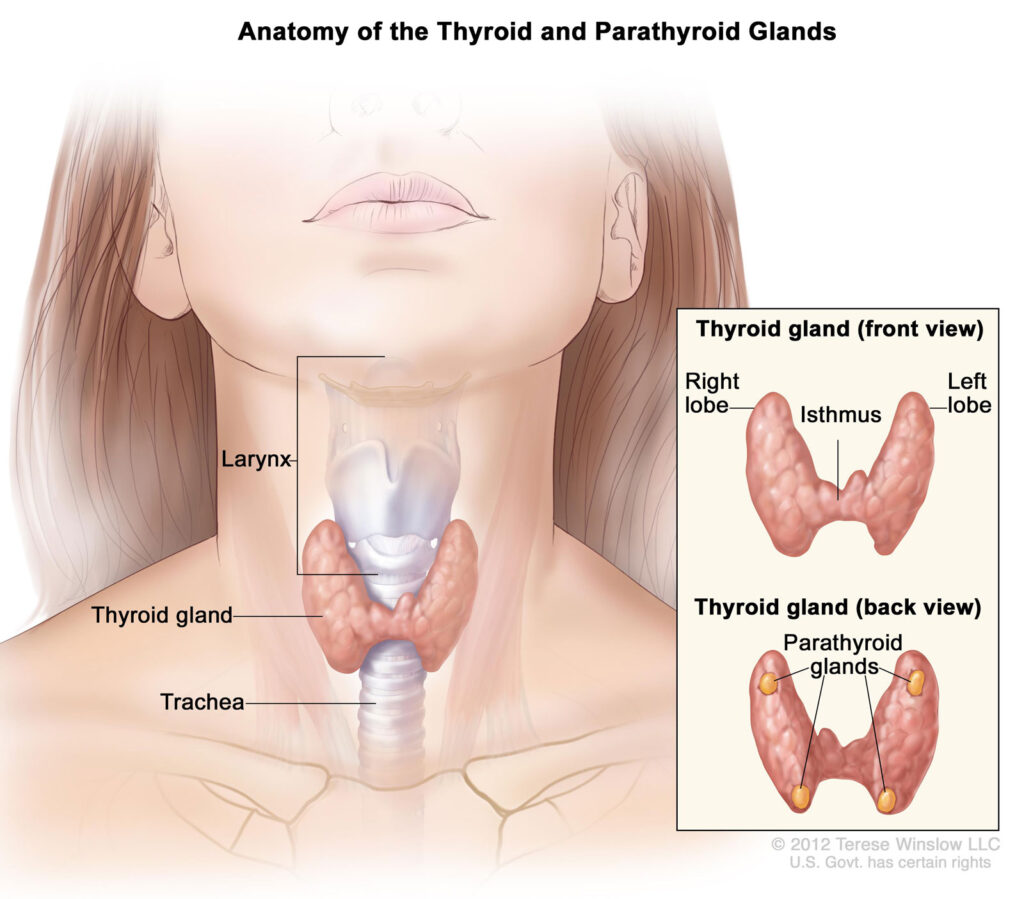
Thyroid surgery, or thyroidectomy, involves the partial or complete removal of the thyroid gland. It is performed to treat a range of conditions including thyroid nodules, hyperthyroidism, goiter, and thyroid cancer. The decision to undergo surgery depends on the nature of the thyroid disorder, its progression, and associated symptoms.
Common Indications for Thyroid Surgery
- Thyroid nodules: Suspicious or malignant nodules confirmed by fine needle aspiration (FNA)
- Thyroid cancer: Papillary, follicular, medullary, or anaplastic carcinoma
- Hyperthyroidism: Especially in cases unresponsive to medication or radioactive iodine
- Goiter: Large or symptomatic multinodular goiter causing airway or swallowing issues
- Thyroid cysts: Recurring or complex cysts not resolving with aspiration
Types of Thyroidectomy Procedures
Thyroidectomy is categorized based on the extent of gland removal. Each approach has specific indications and postoperative implications.
1. Total Thyroidectomy
- Removal of the entire thyroid gland
- Indicated in thyroid cancer, bilateral nodular disease, or Graves’ disease
- Requires lifelong thyroid hormone replacement
2. Hemithyroidectomy (Lobectomy)
- Removal of one lobe of the thyroid
- Common for isolated nodules or indeterminate FNA results
- May not require hormone replacement if remaining lobe functions normally
3. Subtotal (Near-Total) Thyroidectomy
- Leaves a small remnant of thyroid tissue
- Historically used in benign multinodular goiter but now less common
4. Completion Thyroidectomy
- Performed after initial lobectomy when malignancy is found
- Converts partial thyroidectomy into total removal
Preoperative Evaluation and Planning
Thorough evaluation ensures optimal outcomes and minimizes complications.
Diagnostic Assessments:
- Thyroid ultrasound: Evaluates nodule characteristics and lymph node involvement
- FNA biopsy: Determines malignancy risk
- Thyroid function tests (TSH, Free T4): Assesses baseline gland activity
- Laryngoscopy: Checks vocal cord mobility pre-surgery
- CT or MRI: Used when substernal extension or invasion is suspected
Patient Preparation:
- Discuss anesthesia risks, scarring, voice changes, and hormone therapy
- Ensure euthyroid state before surgery
- Consider calcium and vitamin D supplementation for high-risk patients
Surgical Procedure and Intraoperative Considerations
Thyroid surgery is typically performed under general anesthesia. A standard collar incision is made in the lower neck to access the gland.
Key Steps in the Operation:
- Skin incision and retraction
- Identification and preservation of:
- Recurrent laryngeal nerve (RLN)
- Parathyroid glands
- Dissection and removal of thyroid tissue
- Hemostasis and wound closure
Use of Intraoperative Neuromonitoring (IONM):
- Assists in RLN identification
- Reduces risk of vocal cord paralysis
- Standard in high-volume thyroid centers
Postoperative Recovery and Hormonal Management
Recovery from thyroid surgery is generally smooth, with most patients discharged within 24–48 hours.
Immediate Postoperative Monitoring:
- Calcium levels: Hypocalcemia may occur due to parathyroid manipulation
- Voice and breathing: Early signs of RLN injury or airway compromise
- Wound inspection: Monitoring for hematoma or seroma
Long-Term Management:
- Levothyroxine therapy: Required in total thyroidectomy to maintain euthyroid state
- TSH suppression: Used in thyroid cancer cases to prevent recurrence
- Follow-up testing: Includes TSH, thyroglobulin, and imaging as needed
Potential Complications of Thyroid Surgery
While generally safe, thyroidectomy carries potential risks that must be discussed preoperatively.
| Complication | Description | Incidence |
|---|---|---|
| Hypocalcemia | Temporary or permanent | 1–5% (permanent) |
| Vocal cord paralysis | Unilateral or bilateral | ~1% (permanent) |
| Hematoma | Can cause airway obstruction | <1% |
| Infection | Rare due to sterile technique | <1% |
| Thyroid storm | Rare, more likely in uncontrolled hyperthyroidism | Very rare |
Thyroid Surgery for Thyroid Cancer
In cases of confirmed thyroid carcinoma, surgical management is the cornerstone of treatment.
Surgical Approach Based on Cancer Type:
- Papillary/Follicular Cancer: Total thyroidectomy with or without central neck dissection
- Medullary Cancer: Requires total thyroidectomy and lymph node dissection
- Anaplastic Cancer: Often inoperable; palliative resection in select cases
Role of Radioactive Iodine (RAI) Post-Surgery:
- Used to ablate residual thyroid tissue or microscopic disease
- Enhances monitoring using thyroglobulin as a tumor marker
Advances in Minimally Invasive and Robotic Thyroid Surgery
Newer surgical techniques reduce scarring and improve patient satisfaction.
Minimally Invasive Video-Assisted Thyroidectomy (MIVAT):
- Small incision (2–3 cm)
- Limited to small nodules or lobectomies
Transoral Endoscopic Thyroidectomy Vestibular Approach (TOETVA):
- Scarless approach via the mouth
- Gaining popularity in cosmetic-sensitive populations
Robotic Thyroidectomy:
- Performed through remote incisions (axillary or retroauricular)
- Requires specialized training and equipment
Post-Thyroidectomy Lifestyle and Follow-Up Care
Patients can resume most daily activities within 1–2 weeks. Long-term follow-up ensures hormonal balance and early detection of recurrence in cancer patients.
Recommendations:
- Thyroid hormone monitoring every 6–12 months
- Neck ultrasound annually in cancer cases
- Voice therapy if persistent hoarseness
- Calcium supplements if parathyroid function remains impaired
Frequently Asked Questions:
Is thyroid surgery a major operation?
Yes, but it is routinely performed and considered safe when done by experienced surgeons.
Will I need to take medication after thyroidectomy?
If the entire thyroid is removed, lifelong thyroid hormone replacement with levothyroxine is required.
How long does it take to recover from thyroid surgery?
Initial recovery is about 1–2 weeks; full recovery and hormonal stabilization may take several months.
Are there visible scars after thyroid surgery?
A small horizontal neck scar is common, though minimally invasive or robotic methods can reduce visibility.
Can thyroid nodules come back after surgery?
Yes, especially if only part of the thyroid is removed. Periodic monitoring is necessary.
Thyroid surgery remains a vital and effective treatment modality for numerous thyroid disorders, particularly malignancy and symptomatic nodular disease. Advances in surgical technique and perioperative care have significantly reduced complication rates and enhanced patient outcomes. A collaborative, informed approach involving endocrinologists, surgeons, and patients ensures optimal management and long-term health.