The thyroid gland is among the most radiation-sensitive organs in the human body. Even low doses of ionizing radiation can disrupt its function or increase the risk of thyroid malignancies, especially in children and young adults. With increasing exposure from medical imaging, nuclear incidents, and occupational hazards, it is essential to implement robust thyroid radiation protection strategies.

Understanding Thyroid Sensitivity to Radiation
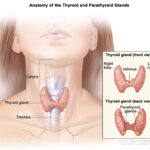
The thyroid gland regulates metabolism by producing hormones such as thyroxine (T4) and triiodothyronine (T3). Radiation affects the thyroid’s DNA, leading to mutations, altered hormone production, and potentially carcinogenesis.
Radiation Effects on the Thyroid:
- Acute effects: Temporary thyroiditis, hormonal imbalances
- Chronic effects: Hypothyroidism, nodular disease, thyroid cancer
Children under 15 years are especially vulnerable, with a significantly higher lifetime risk per unit of radiation dose.
Common Sources of Radiation Exposure to the Thyroid
Understanding the primary sources of exposure is critical for developing protective strategies.
Medical Sources:
- CT scans of the head/neck
- Dental X-rays
- Nuclear medicine procedures (e.g., I-131 therapy)
Environmental and Occupational Sources:
- Nuclear accidents (e.g., Chernobyl, Fukushima)
- Radiologic work environments (healthcare, nuclear plants)
- Space radiation for astronauts
Methods of Thyroid Gland Radiation Protection
A multi-layered approach combining mechanical, pharmacological, and procedural strategies offers the best defense against radiation-induced thyroid damage.
1. Lead Shielding and Protective Collars
Lead-lined thyroid collars and neck shields are essential during diagnostic radiologic procedures.
- Thyroid shield efficacy: Reduces scattered radiation by up to 95%
- Recommended during: Dental X-rays, fluoroscopy, CT scans (when appropriate)
Patients and technicians should ensure correct collar placement to avoid exposure gaps.
2. Iodine Prophylaxis: Potassium Iodide (KI) Administration
KI acts by saturating the thyroid with stable iodine, thereby preventing the uptake of radioactive iodine isotopes (especially I-131).
When to Use KI:
- Before or shortly after exposure
- Most effective within 1–2 hours of exposure
- Dosage depends on age and body weight
WHO Recommended Doses:
| Age Group | KI Dose (mg) |
|---|---|
| Newborns (0–1 month) | 16 mg |
| Infants (1 month–3 years) | 32 mg |
| Children (3–12 years) | 65 mg |
| Adolescents and Adults | 130 mg |
Should be taken only under guidance in nuclear incidents, not as daily prevention.
3. Procedure-Specific Dose Optimization
Technicians and physicians must tailor radiation dose protocols to reduce unnecessary thyroid exposure.
- Low-dose CT techniques
- Collimation and shielding
- Avoiding unnecessary repeat scans
- Non-radiative alternatives: Ultrasound, MRI when appropriate
4. Monitoring and Protective Measures for High-Risk Groups
Healthcare professionals, nuclear industry workers, and patients undergoing repeated imaging require enhanced protective protocols.
- Regular thyroid ultrasounds and TSH testing
- Use of personal dosimeters
- Implementation of ALARA principles (As Low As Reasonably Achievable)
Radiation and Thyroid Cancer Risk: Epidemiological Evidence
Radiation exposure to the thyroid has a well-established link with papillary thyroid carcinoma (PTC), especially following childhood exposure.
Key Data Points:
- Chernobyl survivors: Marked increase in thyroid cancer among exposed children
- Medical imaging: Repeated pediatric CT scans linked to increased thyroid malignancy risk
- Radiotherapy: Patients treated for Hodgkin’s lymphoma or head and neck cancers are at higher secondary thyroid cancer risk
Guidelines and Global Recommendations for Thyroid Radiation Protection
ICRP (International Commission on Radiological Protection)
- Advocates the use of protective devices during all medical procedures involving neck radiation
WHO (World Health Organization)
- Recommends KI distribution in nuclear emergencies
- Emphasizes preparedness in radiation-prone zones
NCRP (National Council on Radiation Protection and Measurements)
- Stresses education and consistent shielding practices across medical facilities
Pediatric Thyroid Protection: A Critical Focus
Children are 10–20 times more sensitive to radiation-induced thyroid cancer compared to adults. For this reason:
- Lead collars must always be used in pediatric imaging
- KI prophylaxis should be prioritized during nuclear events
- Education of caregivers on the risks of unnecessary imaging is essential
Future Innovations in Thyroid Protection
Emerging technologies aim to further reduce radiation exposure:
- AI-based imaging dose modulation
- Wearable smart thyroid shields
- Personalized KI dosing algorithms
- 3D-printed anatomical shields
Protecting the thyroid gland from radiation is not just a clinical obligation—it is a public health imperative. With targeted strategies like shielding, iodine prophylaxis, dose optimization, and education, we can substantially reduce the risks associated with thyroid radiation exposure. The integration of these approaches across clinical and emergency contexts ensures long-term endocrine health and minimizes cancer risk.
Frequently Asked Questions:
What is the best way to protect the thyroid from radiation?
Using a properly fitted lead thyroid collar during radiation exposure and administering potassium iodide in nuclear emergencies are highly effective.
Why is the thyroid so sensitive to radiation?
The thyroid actively concentrates iodine, including radioactive isotopes, which increases its susceptibility to damage from ionizing radiation.
Who should take potassium iodide?
Only individuals at risk of exposure to radioactive iodine, such as during a nuclear accident, should take KI, and only under public health guidance.
Are thyroid collars effective during dental X-rays?
Yes, they significantly reduce scattered radiation to the thyroid and are recommended for both children and adults.
Is thyroid cancer caused by radiation treatable?
Yes, papillary thyroid cancer—most commonly associated with radiation exposure—typically has a high cure rate when detected early.