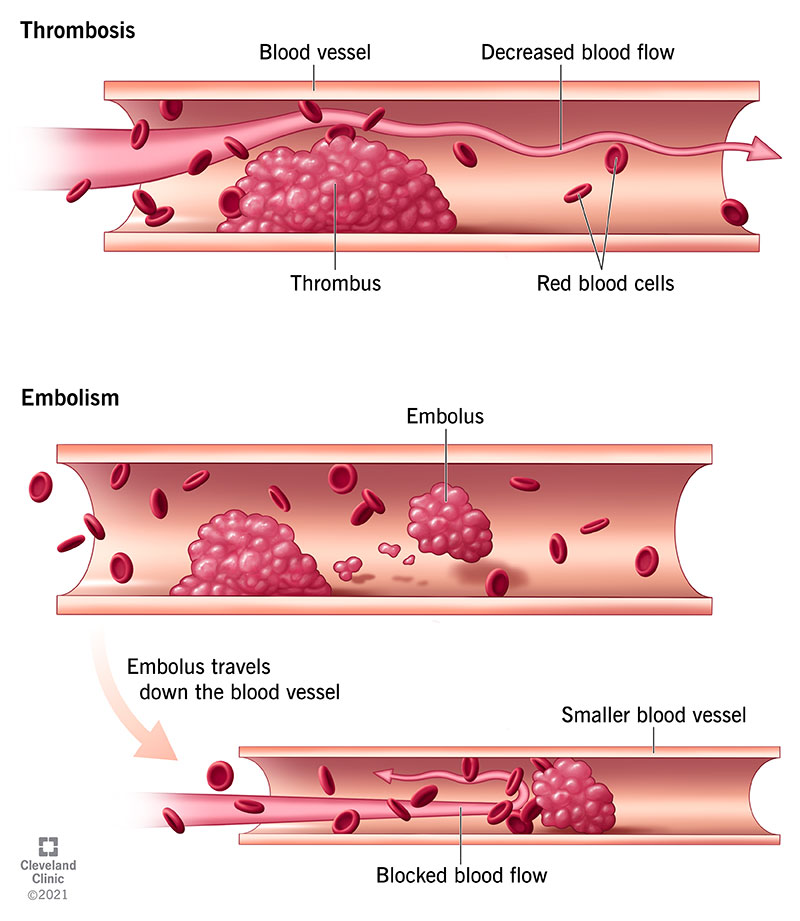
Thrombotic disorders encompass a range of conditions where abnormal blood clot formation—thrombosis—occurs within blood vessels. These disorders pose significant health risks, as clots can obstruct blood flow and cause tissue ischemia or embolism. Thrombosis may occur in veins (venous thrombosis) or arteries (arterial thrombosis), each with distinct causes, risk factors, and consequences.
Classification of Thrombotic Disorders
Venous Thromboembolism (VTE)
VTE includes two main entities:
- Deep Vein Thrombosis (DVT): Clots form in the deep veins, commonly in the legs.
- Pulmonary Embolism (PE): A DVT fragment dislodges and travels to the lungs, blocking pulmonary arteries.
Arterial Thrombosis
Occurs in arteries and is commonly associated with atherosclerosis and cardiovascular disease. It leads to:
- Ischemic stroke
- Myocardial infarction (heart attack)
- Peripheral arterial disease (PAD)
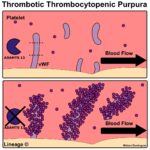
Microvascular Thrombosis
This form involves small vessels and may occur in:
- Thrombotic thrombocytopenic purpura (TTP)
- Disseminated intravascular coagulation (DIC)
- Catastrophic antiphospholipid syndrome (CAPS)
Causes and Risk Factors of Thrombotic Disorders
Genetic and Inherited Factors
- Factor V Leiden mutation
- Prothrombin gene mutation
- Protein C, S, or antithrombin deficiency
- Hyperhomocysteinemia
Acquired Risk Factors
- Immobility and surgery
- Cancer and chemotherapy
- Obesity and smoking
- Oral contraceptives and hormone therapy
- Pregnancy and postpartum state
- Autoimmune diseases (e.g., lupus anticoagulant)
Pathophysiology: The Triad of Thrombosis
Virchow’s Triad explains the three primary mechanisms that promote thrombosis:
- Endothelial injury – Damage to the vessel lining initiates clotting.
- Stasis of blood flow – Reduced flow encourages clot accumulation.
- Hypercoagulability – Increased tendency of the blood to clot.
Clinical Manifestations of Thrombotic Disorders
Signs of Deep Vein Thrombosis (DVT)
- Swelling in one leg
- Pain or tenderness, often in the calf
- Warmth or redness
Symptoms of Pulmonary Embolism (PE)
- Sudden shortness of breath
- Chest pain, especially on deep breathing
- Rapid heartbeat
- Cough, sometimes with bloody sputum
Arterial Thrombosis Symptoms
- Numbness or weakness (stroke)
- Chest pain and arm discomfort (heart attack)
- Claudication or limb pain on exertion (PAD)
Diagnostic Methods for Thrombotic Disorders
Blood Tests
- D-dimer test: Elevated in active thrombosis
- Coagulation profile: PT, aPTT, fibrinogen levels
- Thrombophilia panel: Genetic and protein deficiencies
Imaging Techniques
- Compression ultrasonography: Preferred for DVT
- CT pulmonary angiography: Gold standard for PE
- MRI and MRA: Used in stroke and arterial thrombosis
- Venography or arteriography: Invasive but accurate
Comprehensive Treatment Strategies
Anticoagulation Therapy
- Heparin and low-molecular-weight heparin (LMWH): Immediate action
- Warfarin: Requires INR monitoring
- Direct oral anticoagulants (DOACs): Apixaban, rivaroxaban, dabigatran—commonly used for VTE and atrial fibrillation
Thrombolytic Therapy
Used in high-risk or massive thrombotic events, such as:
- Alteplase (tPA) for PE or stroke
- Administered under close monitoring due to bleeding risks
Surgical and Interventional Options
- Thrombectomy: Mechanical removal of clot
- Inferior vena cava (IVC) filter: For patients with contraindications to anticoagulation
- Angioplasty and stenting: For arterial obstructions
Duration of Anticoagulation
- 3–6 months for provoked DVT/PE
- Extended or lifelong in cases of unprovoked or recurrent thrombosis, or persistent risk factors
Preventive Measures and Risk Reduction
Lifestyle Modifications
- Regular physical activity
- Weight management
- Smoking cessation
- Adequate hydration during travel
Medical Prophylaxis
- LMWH or DOACs in high-risk hospitalized or postoperative patients
- Compression stockings for immobilized patients
- Early ambulation post-surgery
Special Populations and Considerations
Cancer-Associated Thrombosis
Patients with malignancy are at increased risk due to pro-thrombotic tumor secretions, chemotherapy, and immobility. LMWH or DOACs are commonly used.
Pregnancy-Related Thrombosis
Pregnancy creates a hypercoagulable state. LMWH is safe and preferred. Warfarin and DOACs are generally avoided during pregnancy and lactation.
COVID-19 and Thrombosis
COVID-19 has been associated with increased thrombotic complications, necessitating prophylactic anticoagulation protocols in hospitalized patients.
Frequently Asked Questions:
What is the most common thrombotic disorder?
Deep vein thrombosis (DVT) is the most frequently encountered thrombotic condition, particularly in hospitalized or immobile patients.
Are thrombotic disorders hereditary?
Some forms are, especially in patients with Factor V Leiden or Protein C/S deficiency. Genetic testing may be indicated in young patients or those with recurrent clots.
Can thrombotic disorders be prevented?
Yes. Through lifestyle modification, risk factor control, and prophylactic anticoagulation in high-risk scenarios.
What is the role of D-dimer in thrombosis?
It helps exclude thrombosis if normal, particularly in low-risk cases. A positive D-dimer warrants further imaging but is not diagnostic alone.
Is aspirin useful in thrombotic disorders?
Aspirin has a role in arterial thrombosis prevention, such as stroke and heart attack, but is not effective for venous thrombosis.
Thrombotic disorders are complex, multifactorial conditions with potentially fatal consequences. Early recognition, proper classification, risk assessment, and targeted treatment strategies are vital to improving outcomes. With advancements in diagnostics and anticoagulation therapies, we can significantly reduce morbidity and mortality associated with thrombosis across various populations and clinical settings.