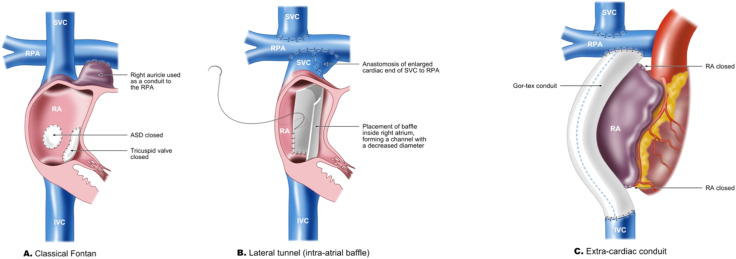
The Fontan procedure is a palliative surgical intervention performed in patients with single-ventricle congenital heart defects. This operation reroutes systemic venous return directly to the pulmonary arteries, bypassing the heart. While it improves oxygenation and survival, it creates a non-pulsatile, low-flow venous circulation that predisposes patients to thrombosis.
Hemodynamic Features Increasing Thrombotic Risk
- Elevated systemic venous pressure
- Low pulmonary blood flow velocity
- Absence of sub-pulmonary ventricle
- Endothelial dysfunction
- Venous stasis
These conditions result in a prothrombotic state, increasing the likelihood of venous thromboembolism (VTE) and intracardiac thrombus formation, which may lead to stroke or pulmonary embolism (PE).
Incidence and Clinical Significance of Thrombosis After Fontan
Thromboembolic events occur in up to 25% of patients following the Fontan procedure. The risk is highest in the first few years post-operation, though long-term surveillance remains essential.
Common Thrombotic Complications
- Pulmonary embolism
- Systemic embolism (e.g., stroke)
- Fontan circuit thrombosis
- Protein-losing enteropathy exacerbation
- Cyanosis due to thrombus-induced flow obstruction
Pathophysiology of Thromboembolism in the Fontan Circuit
The Fontan circulation inherently meets the Virchow’s triad for thrombosis:
- Stasis of blood flow: Reduced cardiac output and passive pulmonary perfusion
- Endothelial injury: Surgical manipulation and chronic venous hypertension
- Hypercoagulability: Protein C and S deficiency, elevated fibrinogen, platelet activation
Risk Stratification for Thromboembolism Post-Fontan
Thrombosis risk varies based on multiple patient-specific and procedural factors.
High-Risk Factors
- Atrial arrhythmias (especially atrial flutter/fibrillation)
- Previous thromboembolic event
- Fenestrated Fontan closure
- Protein-losing enteropathy
- Ventricular dysfunction
- Residual intracardiac shunts
- Central venous catheters
Thrombosis Prevention Strategies After Fontan Procedure
A preventive approach must be individualized based on age, underlying risk, and surgical variations. There is no universal consensus, but strategies are based on clinical evidence and expert guidelines.
1. Antithrombotic Therapy Options
a. Antiplatelet Agents
- Aspirin (3–5 mg/kg/day) is commonly used in low-risk pediatric patients.
- Mechanism: Inhibits platelet aggregation via irreversible COX-1 inhibition.
- Benefits: Well-tolerated, low bleeding risk.
b. Oral Anticoagulants
- Warfarin: Used in high-risk individuals or those with atrial arrhythmias.
- Target INR: 2.0–3.0
- Requires frequent monitoring and dietary consistency
- Direct Oral Anticoagulants (DOACs):
- Agents like rivaroxaban and apixaban are being studied.
- Benefits: Fixed dosing, no routine monitoring.
- Not universally approved in pediatrics or all congenital heart disease types.
c. Combined Therapy
- Some clinicians opt for aspirin plus low-dose warfarin in very high-risk profiles.
- Increases bleeding risk; used cautiously.
2. Mechanical and Lifestyle Measures
- Compression stockings to prevent venous pooling
- Hydration to reduce blood viscosity
- Early ambulation post-surgery
- Avoidance of central venous catheters when possible
Monitoring and Follow-Up
Continuous surveillance is essential for optimal thrombosis prevention.
Recommended Monitoring Protocols
- Regular imaging: Echocardiography, MRI, or CT to evaluate Fontan conduit patency and detect thrombi
- Serial laboratory evaluations:
- INR monitoring for warfarin
- Platelet function and D-dimer (if clinically indicated)
- Holter monitoring for arrhythmias
Current Evidence and Ongoing Research
Despite multiple studies, the optimal antithrombotic regimen remains debated. The PREVENTION trial and other ongoing research aim to clarify whether DOACs can safely replace warfarin or aspirin in this setting.
Summary of Current Consensus
| Risk Level | Recommended Therapy |
|---|---|
| Low Risk | Aspirin monotherapy |
| Moderate Risk | Warfarin or Aspirin |
| High Risk | Warfarin (INR 2–3), ± aspirin |
| Post-thrombotic | Warfarin for ≥6 months, reevaluation |
Special Considerations in Pediatric Patients
- Dosing challenges and limited approval of DOACs in children necessitate cautious use.
- Growth changes affect drug pharmacokinetics.
- Parental education and adherence play a critical role in anticoagulant therapy success.
Thrombosis prevention after the Fontan procedure is an essential element of long-term management. Individualized strategies incorporating clinical risk factors, antithrombotic pharmacotherapy, and close follow-up are critical to minimizing thromboembolic complications. As further research refines our understanding, integrating newer anticoagulants may enhance safety and efficacy in selected patients.