Heparin-induced thrombocytopenia (HIT) is a prothrombotic, immune-mediated adverse reaction to heparin exposure. Paradoxically, HIT causes thrombosis rather than bleeding, despite the hallmark of thrombocytopenia. It typically occurs 4–14 days after initiation of heparin and can lead to arterial or venous thromboembolism, making it a hematologic emergency requiring immediate intervention.
Pathophysiology of HIT-Associated Thrombosis
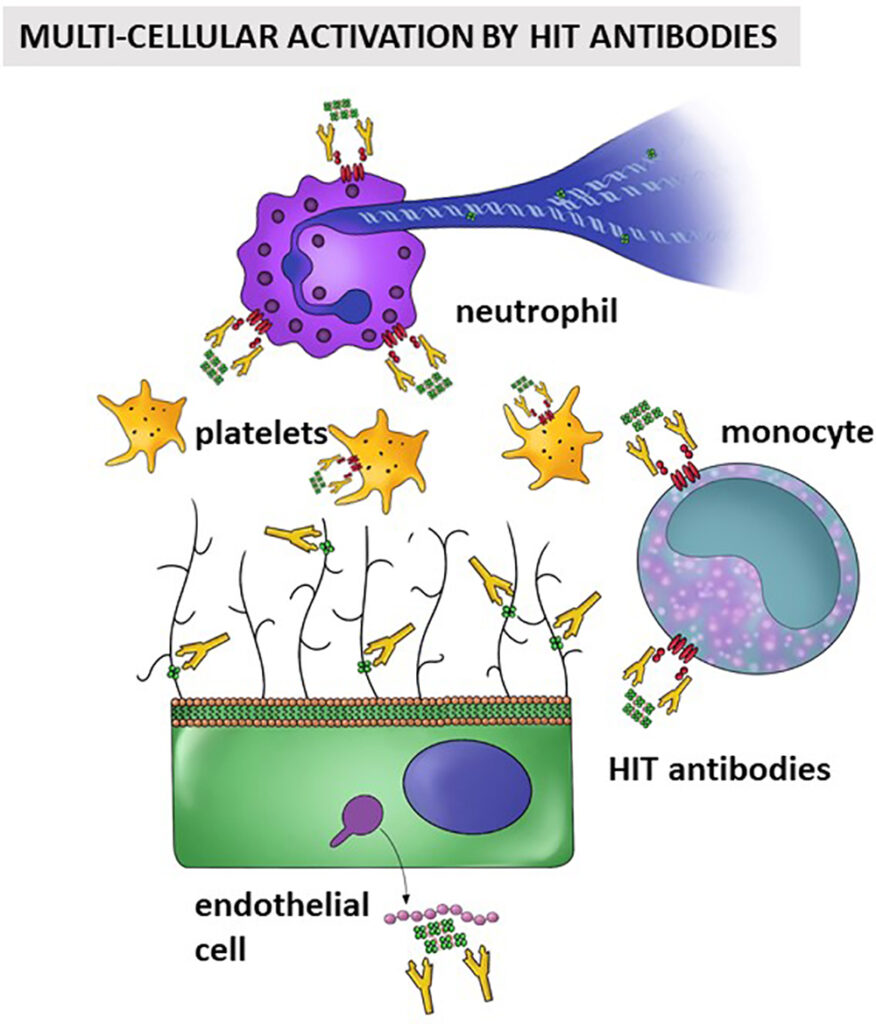
Thrombosis in HIT is triggered by an immune complex formed between platelet factor 4 (PF4) and heparin, which in turn binds to IgG antibodies. These immune complexes activate platelets via the FcγIIa receptor, promoting massive thrombin generation.
Key Steps in HIT-Driven Thrombosis
- Heparin binds to PF4 released from platelet α-granules.
- Immune response generates IgG antibodies against PF4-heparin complexes.
- These immune complexes crosslink platelets, activating them.
- Procoagulant microparticles are released.
- Endothelial cells and monocytes are activated, amplifying thrombosis.
- Disseminated thrombosis may occur despite low platelet counts.
Clinical Presentation of HIT with Thrombosis
Up to 50% of HIT cases develop thrombotic complications—a condition known as HITT (heparin-induced thrombocytopenia with thrombosis). These events often occur before or during the detection of thrombocytopenia.
Common Thrombotic Manifestations
- Deep vein thrombosis (DVT)
- Pulmonary embolism (PE)
- Arterial thrombosis (e.g., limb ischemia, stroke, myocardial infarction)
- Skin necrosis at heparin injection sites
- Adrenal hemorrhagic infarction
- Disseminated intravascular coagulation (DIC) (rare but severe)
Risk Factors and Types of Heparin Involved
Risk Factors
- Unfractionated heparin (UFH): Highest incidence
- Surgical patients, particularly orthopedic and cardiac
- Female sex
- Prolonged heparin exposure
- Previous HIT history
HIT Types
- Type I HIT: Non-immune, transient, benign (early-onset)
- Type II HIT: Immune-mediated, delayed onset, associated with thrombosis
| Heparin Type | Thrombosis Risk | HIT Risk |
|---|---|---|
| Unfractionated Heparin | High | High |
| Low Molecular Weight Heparin (LMWH) | Moderate | Lower |
| Fondaparinux | Negligible | Rare |
Diagnostic Evaluation
1. Clinical Scoring: The 4T’s Score
| Criteria | 2 points | 1 point | 0 points |
|---|---|---|---|
| Thrombocytopenia | >50% fall, nadir ≥20k | 30–50% fall or nadir 10–19k | <30% fall or nadir <10k |
| Timing of Platelet Fall | Days 5–10 | After day 10 | <Day 4 or inconsistent |
| Thrombosis | Proven new thrombosis | Progressive/recurrent thrombosis | No thrombosis |
| Other causes | None apparent | Possible | Definite |
Score ≥6: High probability
Score 4–5: Intermediate
Score ≤3: Low probability
2. Laboratory Testing
Immunoassays
- ELISA for PF4-heparin antibodies
- High sensitivity but not always specific
Functional Assays
- Serotonin Release Assay (SRA) – gold standard
- Heparin-induced Platelet Activation (HIPA) test
Management of HIT with Thrombosis
Immediate cessation of all forms of heparin is mandatory—even flushes or coated catheters. Anticoagulation must not be delayed, even if platelet counts are low.
Stepwise Approach to Treatment
- Discontinue Heparin Immediately
- Initiate Non-Heparin Anticoagulant
- Direct Thrombin Inhibitors:
- Argatroban
- Bivalirudin
- Factor Xa Inhibitors:
- Fondaparinux
- Rivaroxaban, Apixaban (oral)
- Direct Thrombin Inhibitors:
- Avoid Platelet Transfusions unless life-threatening hemorrhage occurs.
- Monitor Platelet Recovery (typically within 7 days).
- Bridge to Warfarin only after platelet count >150,000/μL.
- Use overlap therapy for ≥5 days and INR >2 on two consecutive days.
Long-Term Management and Follow-Up
Duration of Anticoagulation
- HIT without thrombosis: Minimum 4 weeks
- HIT with thrombosis (HITT): 3–6 months
Warfarin Considerations
- Avoid initiating during acute HIT due to risk of warfarin-induced skin necrosis and limb gangrene.
- Ensure platelet count recovery before initiating.
Monitoring and Secondary Prevention
- Detailed documentation of HIT diagnosis in patient records
- Avoidance of all heparin forms in future care
- Use of medical alert bracelets or cards
Complications and Prognosis
Without prompt diagnosis and treatment, thrombosis in HIT can result in:
- Amputation
- Severe ischemic strokes
- Multiorgan failure
- Death
Mortality rate in untreated HIT with thrombosis can approach 20–30%. With effective management, outcomes improve significantly, and recurrence is rare if heparin is avoided.
Thrombosis in heparin-induced thrombocytopenia is a critical prothrombotic disorder requiring high clinical vigilance. Timely identification, immediate heparin cessation, and initiation of alternative anticoagulation are the cornerstones of management. Understanding the immune-mediated mechanism, using structured diagnostic tools like the 4T’s score, and selecting appropriate non-heparin anticoagulants significantly reduce morbidity and mortality in affected patients.