Thrombocytopenia is a common hematologic manifestation in patients with chronic hepatitis C virus (HCV) infection. It is characterized by a platelet count below 150,000/µL and is often multifactorial in origin. As the disease progresses, thrombocytopenia becomes more prominent, particularly in the context of cirrhosis and portal hypertension. Its presence may serve as both a marker of liver disease severity and a clinical barrier to the initiation and continuation of antiviral therapy or invasive diagnostic procedures.
Pathophysiology: Mechanisms of HCV-Induced Thrombocytopenia
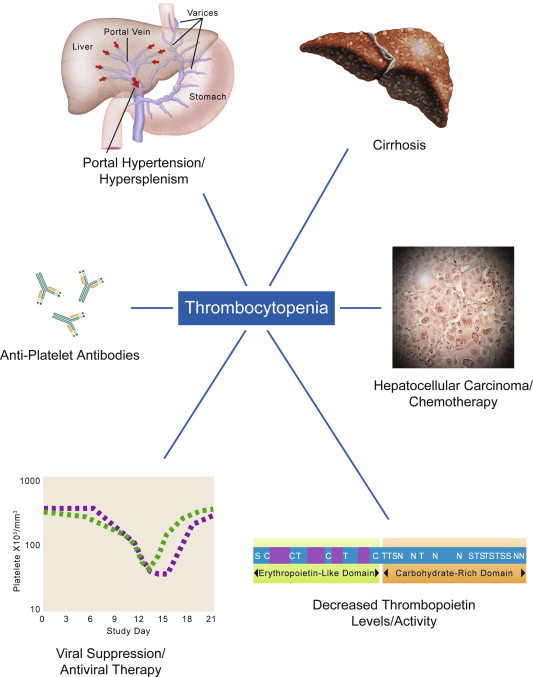
1. Splenic Sequestration Due to Portal Hypertension
Chronic HCV infection often results in liver fibrosis and cirrhosis, leading to increased resistance in the portal circulation. This elevated pressure contributes to splenomegaly, where the enlarged spleen retains and destroys platelets at an accelerated rate.
2. Decreased Thrombopoietin Production
The liver is the primary site for thrombopoietin (TPO) synthesis, a hormone critical for platelet production. Hepatocellular damage in HCV diminishes TPO output, impairing megakaryocyte development and platelet generation.
3. Bone Marrow Suppression
HCV has been shown to exert a direct suppressive effect on the bone marrow. Moreover, interferon-based therapies used historically to treat HCV exacerbate cytopenias, including thrombocytopenia, by reducing hematopoietic activity.
4. Autoimmune-Mediated Platelet Destruction
HCV infection is associated with the development of autoantibodies against platelets. This immune-mediated destruction is a significant contributor to thrombocytopenia, particularly in early stages of the disease before cirrhosis develops.
5. Antiviral Therapy-Induced Cytopenia
Although modern direct-acting antivirals (DAAs) have greatly reduced hematologic toxicity, legacy interferon and ribavirin regimens are linked with significant decreases in platelet counts, necessitating dose modifications or treatment discontinuation.
Clinical Significance of Thrombocytopenia in HCV Patients
1. Impaired Antiviral Treatment Delivery
Low platelet counts can delay or limit the administration of antiviral drugs, particularly interferon-based therapies. Though DAAs are better tolerated, extremely low platelet counts still pose treatment challenges in some patients.
2. Increased Bleeding Risk
Thrombocytopenia elevates the risk of bleeding, particularly during procedures such as liver biopsy, endoscopy, or surgery. Gastrointestinal hemorrhages are of particular concern in patients with esophageal varices.
3. Diagnostic Limitations
Invasive diagnostics that are critical for assessing liver fibrosis or hepatocellular carcinoma may be postponed or avoided due to bleeding risk, impacting timely diagnosis and management.
Diagnostic Approach to Thrombocytopenia in HCV
1. Complete Blood Count (CBC)
Initial evaluation includes determining platelet count and examining red and white blood cell indices. Pancytopenia may suggest hypersplenism or bone marrow suppression.
2. Liver Function Tests (LFTs)
Elevation in transaminases, bilirubin, and prothrombin time supports ongoing hepatic injury or decompensation.
3. Abdominal Ultrasound
Evaluates liver morphology, splenic size, and the presence of ascites or varices suggestive of portal hypertension.
4. Thrombopoietin Level
Low levels may confirm decreased hepatic production and guide decisions about using thrombopoietin receptor agonists.
5. Autoantibody Testing
Helps identify autoimmune thrombocytopenia in patients presenting with early-stage HCV or without cirrhosis.
6. Bone Marrow Biopsy
Indicated when the etiology remains unclear or if there is evidence of aplastic anemia, myelodysplasia, or other marrow disorders.
Management and Treatment of HCV-Associated Thrombocytopenia
1. Direct-Acting Antiviral Therapy (DAAs)
Modern DAA regimens such as sofosbuvir/velpatasvir or glecaprevir/pibrentasvir achieve sustained virologic response (SVR) in over 95% of cases and are associated with significant improvement in platelet counts. Viral clearance reduces hepatic inflammation, improves TPO synthesis, and alleviates splenic sequestration.
2. Thrombopoietin Receptor Agonists (TPO-RAs)
TPO-RAs stimulate platelet production and are particularly effective in patients who require short-term platelet elevation prior to procedures.
| Agent | Route | Use Case | Approval Status |
|---|---|---|---|
| Eltrombopag | Oral | Chronic ITP, HCV-associated thrombocytopenia | FDA approved |
| Avatrombopag | Oral | Pre-procedure platelet increase | FDA approved |
| Lusutrombopag | Oral | Perioperative support in CLD | FDA approved |
3. Platelet Transfusions
Used acutely in patients with active bleeding or those undergoing invasive procedures. Effects are transient and often inadequate as a standalone strategy.
4. Corticosteroids and IVIG
Immunosuppressive therapies may benefit patients with immune-mediated thrombocytopenia. However, their role in HCV-related cases remains limited and often adjunctive.
5. Splenectomy
Reserved for refractory thrombocytopenia where hypersplenism is the predominant cause. Risks include postsplenectomy sepsis and thrombosis, and the procedure is rarely first-line.
Preventive Strategies and Monitoring
1. Regular Monitoring of Platelet Count
Frequent CBC testing is necessary during antiviral therapy, especially in patients with advanced fibrosis or cirrhosis.
2. Avoidance of Hepatotoxic Agents
NSAIDs, alcohol, and herbal supplements that impair liver function must be avoided to prevent further thrombocytopenia.
3. Vaccination
Patients with chronic HCV should receive hepatitis A and B vaccines if not already immune, reducing the risk of superinfection and hepatic decompensation.
4. Nutritional Optimization
Micronutrient deficiencies, especially folate and B12, should be corrected to support hematologic recovery.
Prognosis and Long-Term Outcomes
Patients achieving SVR with DAAs often experience resolution or significant improvement of thrombocytopenia over time. The degree of platelet recovery is closely linked to hepatic regeneration and reduction in portal pressure. However, in patients with decompensated cirrhosis or splenic pathology, thrombocytopenia may persist and require ongoing supportive care.
Thrombocytopenia associated with chronic hepatitis C is a multifactorial complication that significantly impacts disease management. Understanding its mechanisms—ranging from splenic sequestration to autoimmune destruction—is critical for guiding diagnosis and treatment. Modern therapies, particularly DAAs and TPO-RAs, have revolutionized patient outcomes, offering safe and effective options for platelet restoration and viral eradication. A comprehensive, individualized approach ensures optimal care and minimizes complications in this complex clinical scenario.