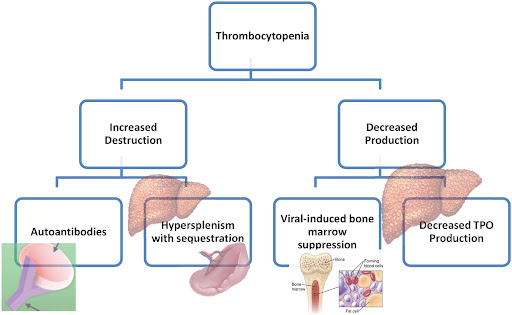
Thrombocytopenia, defined as a platelet count below 150,000/µL, is a frequent hematological abnormality in patients with chronic hepatitis. It is most commonly observed in those with chronic hepatitis B (CHB), chronic hepatitis C (CHC), and advanced liver disease such as cirrhosis. The condition results from a multifactorial pathogenesis involving hypersplenism, impaired thrombopoietin (TPO) production, bone marrow suppression, and autoimmune mechanisms.
This complication not only reflects disease severity but also poses challenges in the management of liver biopsy, antiviral therapy, and invasive procedures. Early recognition and appropriate intervention are essential to mitigate bleeding risks and optimize therapeutic outcomes.
Etiopathogenesis of Thrombocytopenia in Chronic Hepatitis
1. Splenic Sequestration and Portal Hypertension
Chronic liver disease often leads to portal hypertension, causing splenomegaly. An enlarged spleen sequesters and prematurely destroys circulating platelets.
2. Reduced Thrombopoietin Production
The liver is the primary site of thrombopoietin synthesis. Chronic hepatocyte injury impairs TPO production, reducing megakaryocyte stimulation and platelet generation in the bone marrow.
3. Bone Marrow Suppression
Hepatitis C virus (HCV) has direct myelosuppressive effects. Additionally, interferon-based therapies further depress bone marrow function, leading to decreased platelet output.
4. Autoimmune Mechanisms
Autoantibodies against platelets, frequently seen in HCV-related immune dysfunction, contribute to peripheral platelet destruction.
5. Antiviral Therapy-Related Effects
Interferon and ribavirin, historically used for hepatitis C, are associated with cytopenias, including thrombocytopenia. Although newer direct-acting antivirals (DAAs) show a better safety profile, careful monitoring remains vital.
Clinical Implications and Associated Risks
1. Bleeding Complications
Patients with severe thrombocytopenia (<50,000/µL) are at high risk for spontaneous bleeding, especially mucosal and gastrointestinal hemorrhage.
2. Procedural Contraindications
Low platelet counts may necessitate transfusion support before invasive interventions such as liver biopsy, endoscopy, or surgery.
3. Antiviral Therapy Delays
Treatment initiation may be delayed or interrupted due to hematological toxicity, affecting virological response and disease progression.
Diagnostic Evaluation of Thrombocytopenia in Hepatitis
A comprehensive assessment is crucial to identify the underlying cause and rule out alternative etiologies.
1. Complete Blood Count (CBC)
Establishes the degree of thrombocytopenia and checks for associated anemia or leukopenia.
2. Liver Function Tests
Elevations in AST, ALT, and bilirubin suggest ongoing hepatic inflammation and dysfunction.
3. Ultrasound with Doppler
Assesses splenomegaly and signs of portal hypertension.
4. Thrombopoietin Level
Helps differentiate central (bone marrow) vs peripheral (destruction/sequestration) causes.
5. Bone Marrow Aspiration (If Indicated)
Performed when the diagnosis is uncertain or pancytopenia is present.
6. Virological Markers
Hepatitis B surface antigen (HBsAg), HCV RNA levels, and viral load monitoring guide the treatment strategy.
Treatment Strategies for Thrombocytopenia in Chronic Hepatitis
Management focuses on addressing the underlying liver disease, improving platelet count, and preventing complications.
1. Antiviral Therapy
- HCV: Direct-acting antivirals (e.g., sofosbuvir/velpatasvir) are associated with significant improvements in platelet count post-treatment.
- HBV: Nucleos(t)ide analogues such as entecavir or tenofovir help reduce liver inflammation and may improve thrombopoiesis over time.
2. Thrombopoietin Receptor Agonists (TPO-RAs)
These agents stimulate megakaryocyte proliferation and platelet production.
| Drug | Mechanism | Indication |
|---|---|---|
| Eltrombopag | Oral non-peptide TPO-RA | HCV-related thrombocytopenia |
| Romiplostim | Subcutaneous peptide TPO-RA | Severe immune thrombocytopenia |
| Avatrombopag / Lusutrombopag | Approved for peri-procedural use | Patients with chronic liver disease undergoing invasive procedures |
3. Platelet Transfusion
Reserved for acute bleeding or as prophylaxis before high-risk procedures. Not a long-term solution due to alloimmunization risk.
4. Splenectomy
Considered in refractory cases where splenic sequestration is the dominant mechanism. Associated with risk of infection and thrombosis.
5. Corticosteroids or IVIG
Used in autoimmune-mediated thrombocytopenia, though efficacy in viral hepatitis-related cases remains limited.
Preventive Measures and Monitoring
1. Routine Surveillance
Regular CBC and liver panel evaluations are essential during and after antiviral therapy.
2. Vaccination
All hepatitis patients should receive hepatitis A and B vaccines if non-immune to prevent superinfection.
3. Avoidance of Hepatotoxic Drugs
NSAIDs, alcohol, and other hepatotoxic agents should be strictly avoided to prevent worsening liver injury and associated cytopenias.
4. Nutritional Support
Adequate protein and vitamin intake (especially B12 and folate) supports hematopoiesis and immune modulation.
Prognosis and Outcomes
With effective antiviral therapy and supportive measures, thrombocytopenia in chronic hepatitis is often reversible. Achieving sustained virological response (SVR) in HCV or viral suppression in HBV correlates with improved platelet counts and reduced bleeding risks. Persistent thrombocytopenia may indicate advanced fibrosis or cirrhosis and warrants hepatology referral.
Thrombocytopenia associated with chronic hepatitis represents a complex interplay of impaired platelet production, sequestration, and immune destruction. Timely identification, appropriate use of antiviral agents, and adjunct therapies such as TPO-RAs enable safe and effective management. A tailored, multidisciplinary approach ensures improved outcomes and minimizes the risk of complications in patients with chronic viral liver disease.

