Thick bronchial secretions refer to abnormally viscous mucus accumulating within the bronchial tubes. These secretions are typically composed of water, glycoproteins, lipids, and immune cells. Under normal conditions, mucus traps inhaled particles and pathogens, and cilia on the bronchial lining help expel it. However, when mucus becomes thick and sticky, it hinders clearance, leading to airway obstruction, bacterial colonization, and chronic inflammation.
Causes of Thick Bronchial Secretions
Numerous underlying factors contribute to the excessive production or abnormal viscosity of bronchial secretions. These include:
1. Chronic Obstructive Pulmonary Disease (COPD)
In COPD, chronic bronchitis leads to hypersecretion of mucus and ciliary dysfunction. Thick secretions are a hallmark, causing persistent cough and airflow limitation.
2. Cystic Fibrosis
This genetic disorder affects chloride channels, resulting in dehydrated, tenacious mucus. Secretions clog airways and promote recurrent infections.
3. Asthma
Asthma involves airway inflammation and increased mucus production, especially during exacerbations, leading to wheezing and productive cough.
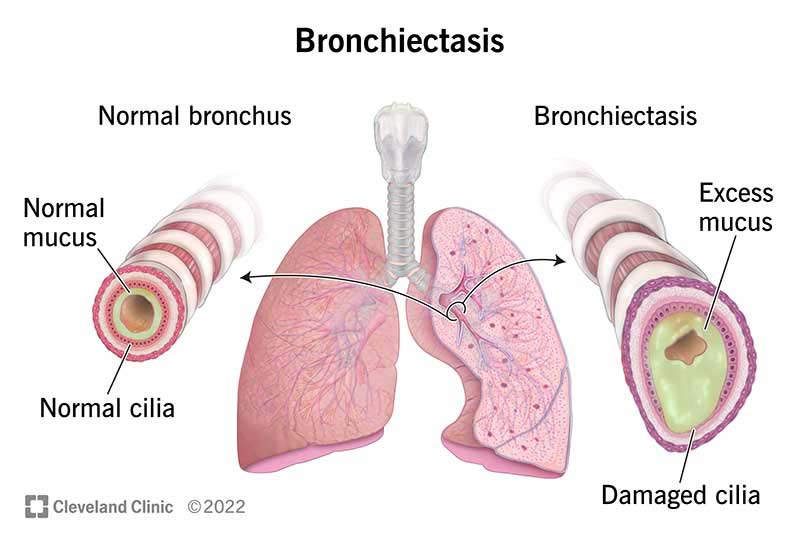
4. Bronchiectasis
This condition features irreversible bronchial dilation, impaired mucus clearance, and chronic infection, often producing large volumes of thick sputum.
5. Respiratory Infections
Bacterial or viral infections, such as pneumonia or influenza, can cause temporary overproduction and thickening of mucus.
6. Dehydration
Insufficient fluid intake decreases mucus hydration, making it more viscous and difficult to expectorate.
7. Environmental Irritants
Exposure to pollutants, tobacco smoke, or occupational dust stimulates mucus hypersecretion and impairs mucociliary function.
Symptoms Associated with Thick Bronchial Secretions
| Symptom | Description |
|---|---|
| Persistent Productive Cough | Often producing yellow, green, or brown sputum |
| Chest Congestion | Sensation of fullness due to mucus accumulation |
| Wheezing and Dyspnea | Resulting from airflow obstruction |
| Crackles on Auscultation | Indicative of mucus in airways |
| Foul-Smelling Sputum | Suggestive of bacterial infection |
Persistent symptoms require thorough evaluation to prevent complications such as pneumonia, atelectasis, or respiratory failure.
Diagnostic Approach to Thick Mucus in Lungs
Effective diagnosis relies on clinical evaluation, imaging, and sputum analysis.
1. Medical History and Physical Examination
- Cough duration, color and volume of sputum
- History of smoking or respiratory conditions
- Lung auscultation for crackles or rhonchi
2. Chest Imaging
- Chest X-ray: Identifies infiltrates or bronchial wall thickening
- CT Scan: Reveals bronchiectasis, mucus plugging, and structural changes
3. Pulmonary Function Tests
Assesses airway obstruction and reversibility in conditions like asthma or COPD.
4. Sputum Culture and Gram Stain
Identifies pathogens contributing to purulent or foul-smelling secretions.
5. Sweat Chloride Test / Genetic Testing
For suspected cystic fibrosis in pediatric or atypical adult cases.
Pathophysiology: How Mucus Becomes Pathologically Thick
Mucus viscosity increases when there is an imbalance in water content, mucin glycoproteins, and ionic transport. Normally, cilia move a thin layer of mucus toward the pharynx. When mucus becomes hyperconcentrated, it adheres to the epithelium, impairing clearance and trapping bacteria, leading to chronic inflammation.
Complications of Untreated Thick Secretions
If not managed, thick bronchial secretions can cause:
- Mucus plugging and atelectasis
- Recurrent pulmonary infections
- Chronic hypoxia
- Bronchial wall remodeling
- Respiratory failure in advanced disease
Prompt management can prevent these serious outcomes.
Treatment and Management of Thick Bronchial Secretions
1. Hydration
Adequate oral or intravenous fluids help thin mucus and improve its clearance.
2. Mucolytics
Medications that chemically break down mucus to reduce viscosity.
Common Mucolytics:
| Drug | Mechanism |
|---|---|
| N-acetylcysteine (NAC) | Breaks disulfide bonds in mucin |
| Dornase alfa | Enzyme targeting DNA in secretions (used in CF) |
| Hypertonic saline | Draws water into mucus via osmotic effect |
3. Airway Clearance Techniques
- Chest physiotherapy (CPT): Percussion and postural drainage
- Oscillatory PEP devices: Loosen mucus through vibrations
- High-frequency chest wall oscillation: Common in cystic fibrosis
- Incentive spirometry: Encourages deep breathing and airway expansion
4. Bronchodilators
Inhaled β2-agonists like albuterol enhance airway patency and facilitate mucus clearance.
5. Antibiotics
Indicated when infection is present or in chronic bronchiectasis to reduce bacterial load.
6. Inhaled Corticosteroids
Used in asthma or COPD to reduce inflammation and mucus hypersecretion.
Preventive Strategies and Long-Term Management
1. Smoking Cessation
Eliminates a major cause of chronic mucus production and ciliary damage.
2. Allergen and Pollution Control
Minimizing environmental triggers through air purifiers, masks, or relocation in severe cases.
3. Vaccination
- Influenza and pneumococcal vaccines help reduce respiratory infections.
- Preventative measures are vital in high-risk populations.
4. Nutritional Support
Adequate caloric and vitamin intake supports immune function and lung health.
5. Regular Pulmonary Follow-up
Chronic conditions require continuous monitoring by pulmonologists to prevent disease progression.
Special Considerations by Age Group
Pediatric Patients
- Often present with cystic fibrosis or viral bronchiolitis.
- Airway clearance and enzyme replacement therapies are essential.
Elderly Patients
- More prone to aspiration and weak cough reflex.
- Need aggressive pulmonary hygiene and swallowing assessments.
When to Seek Immediate Medical Attention
Medical evaluation is warranted if the following occur:
- High fever with productive cough
- Blood-streaked or foul-smelling sputum
- Difficulty breathing or cyanosis
- Significant drop in oxygen saturation
- Symptoms persist despite treatment
Proactive Management Prevents Complications
Thick bronchial secretions are a clinical challenge across various respiratory disorders. With early identification, targeted therapy, and diligent airway clearance strategies, patients can maintain optimal lung function and avoid serious complications. A comprehensive approach integrating pharmacologic, mechanical, and lifestyle interventions is essential for long-term success.