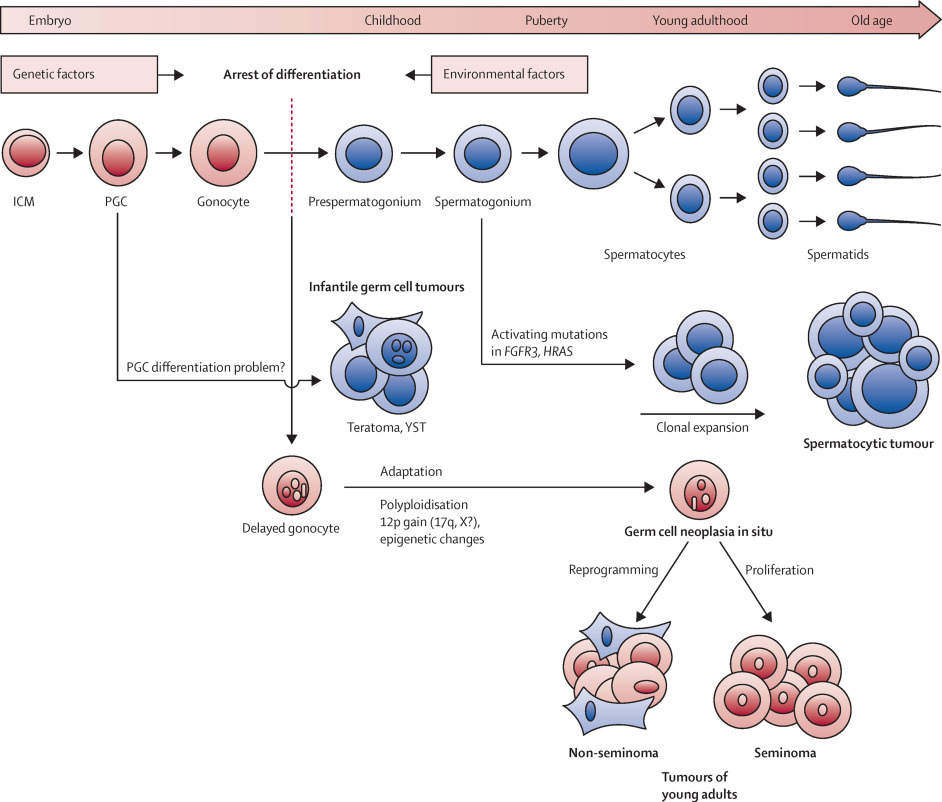
Testicular germ cell tumors (TGCTs) represent the most common form of testicular cancer, predominantly affecting males between the ages of 15 and 40. Derived from the primordial germ cells of the testes, these malignancies are typically highly curable with prompt diagnosis and appropriate treatment. Germ cell tumors account for approximately 95% of all testicular malignancies, and are classified into two broad categories: seminomas and non-seminomas.
Classification of Testicular Germ Cell Tumors
Testicular germ cell tumors are histologically categorized based on their differentiation:
Seminomas
- Typically arise in men aged 30–50.
- Grow slowly and are highly sensitive to radiation and chemotherapy.
- Uniform histology and elevated placental alkaline phosphatase (PLAP).
Non-Seminomas
- More aggressive and occur earlier, between 20–30 years of age.
- Often present with elevated tumor markers.
- Can include one or more histological subtypes such as:
- Embryonal carcinoma: Highly malignant, often mixed with other types.
- Yolk sac tumor: Most common in children; elevated AFP.
- Choriocarcinoma: Highly vascular and metastatic.
- Teratoma: Composed of multiple tissue types; may be benign or malignant.
Risk Factors for Testicular Germ Cell Tumors
Several genetic and environmental factors increase the likelihood of developing TGCTs:
- Cryptorchidism (undescended testicle)
- Family history of testicular cancer
- Personal history of TGCT in the contralateral testis
- Klinefelter syndrome
- Infertility and subfertility
- Exposure to endocrine disruptors during fetal development
Clinical Presentation and Symptoms
Most patients discover the tumor as a painless lump or swelling in the testis. However, additional signs and symptoms may include:
- Scrotal heaviness or discomfort
- Gynecomastia (increased breast tissue, especially in hCG-producing tumors)
- Back pain or abdominal mass (in case of retroperitoneal metastasis)
- Cough, hemoptysis, or dyspnea (lung metastases)
- Neurological symptoms (brain metastases in rare cases)
Diagnostic Approach
Physical Examination
A thorough testicular and abdominal exam is critical to identify any masses or lymphadenopathy.
Tumor Markers
Tumor markers aid in diagnosis, staging, and monitoring response to therapy:
| Marker | Associated Tumor Type | Clinical Significance |
|---|---|---|
| AFP | Yolk sac tumor, embryonal | Should not be elevated in seminoma |
| hCG | Choriocarcinoma, seminoma | May lead to gynecomastia |
| LDH | Non-specific | Correlates with tumor burden |
Imaging
- Scrotal Ultrasound: Primary modality for evaluating testicular masses
- CT Abdomen and Chest: For staging and identifying metastatic spread
- MRI Brain: If neurological symptoms are present
Staging of Testicular Germ Cell Tumors
Staging follows the American Joint Committee on Cancer (AJCC) TNM system:
- T (Tumor size and invasion)
- N (Lymph node involvement)
- M (Distant metastasis)
- S (Serum tumor markers)
Stage Grouping:
- Stage I: Confined to the testis
- Stage II: Spread to retroperitoneal lymph nodes
- Stage III: Distant metastases (lungs, liver, brain, etc.)
Treatment Strategies
Treatment depends on tumor type, stage, and patient factors. Management typically involves a multidisciplinary approach.
Radical Inguinal Orchiectomy
- First-line treatment for all suspected TGCTs.
- Trans-scrotal biopsy is contraindicated due to the risk of tumor seeding.
Additional Therapies by Tumor Type
Seminomas:
| Stage | Treatment |
|---|---|
| I | Surveillance, radiation, or chemotherapy |
| II | Radiotherapy or chemotherapy |
| III | Chemotherapy (e.g., BEP regimen) |
Non-Seminomas:
| Stage | Treatment |
|---|---|
| I | Surveillance or adjuvant chemotherapy |
| II | Retroperitoneal lymph node dissection (RPLND) or chemotherapy |
| III | Chemotherapy followed by RPLND if residual mass exists |
Chemotherapy Regimens
- BEP (Bleomycin, Etoposide, Cisplatin) is the gold standard.
- Administered in cycles depending on disease stage.
Prognosis and Survival Rates
Prognosis is highly favorable with timely intervention:
| Stage | 5-Year Survival Rate |
|---|---|
| Stage I | >99% |
| Stage II | 96%–98% |
| Stage III | 74%–95% |
Prognosis is guided by International Germ Cell Consensus Classification (IGCCC):
- Good: No non-pulmonary visceral metastasis
- Intermediate: Non-seminomatous tumors with moderate tumor markers
- Poor: High tumor burden with liver/brain metastases or very high markers
Follow-Up and Surveillance
Long-term follow-up is essential for early detection of recurrence or treatment-related complications.
- Physical exams and tumor marker evaluation every 3–6 months
- Imaging studies (CT or chest X-ray) periodically
- Monitor for secondary malignancies and chemotherapy toxicity
Prevention and Self-Examination
While TGCTs cannot always be prevented, early detection greatly enhances prognosis. Monthly testicular self-examinations are recommended for high-risk individuals.
Self-Examination Steps:
- After a warm shower, stand in front of a mirror.
- Check for swelling or visual abnormalities.
- Roll each testicle gently between the fingers.
- Report any hard lumps, irregularities, or pain to a physician promptly.
Frequently Asked Questions:
Are all testicular germ cell tumors cancerous?
Yes, TGCTs are malignant. However, some subtypes such as mature teratomas may behave benignly but still require removal.
Can testicular cancer recur after treatment?
Yes. Recurrence is possible, especially within the first 2 years. Surveillance is critical.
Is fertility affected by treatment?
Chemotherapy and surgery may affect fertility. Sperm banking is recommended before treatment initiation.
Do TGCTs spread to other organs?
Yes. The lungs, liver, brain, and lymph nodes are common metastatic sites in advanced stages.
Can testicular germ cell tumors be cured?
Yes, cure rates exceed 95%, especially with early-stage detection and treatment.
Testicular germ cell tumors are highly treatable malignancies when addressed promptly. A structured approach involving early diagnosis, surgical intervention, and systemic therapy ensures optimal outcomes. Ongoing advancements in treatment protocols and vigilant post-treatment monitoring continue to improve survival rates. Awareness, early detection, and patient education remain essential pillars in managing this potentially curable cancer.