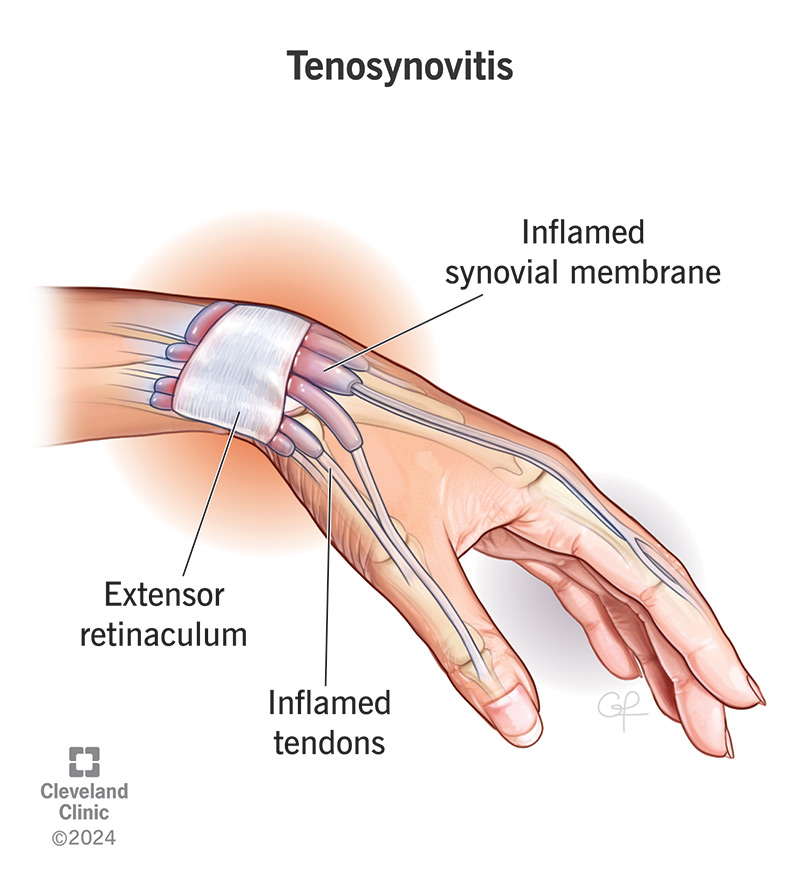
Tenosynovitis is the inflammation of the synovial sheath, the thin layer of tissue that surrounds tendons. It typically occurs in areas where tendons pass through narrow anatomical tunnels, particularly in the hands, wrists, feet, and ankles. The condition can result in pain, swelling, restricted movement, and in severe cases, tendon damage.
Unlike general tendonitis, which involves inflammation of the tendon itself, tenosynovitis primarily affects the protective sheath surrounding the tendon, although both conditions may coexist.
Common Types of Tenosynovitis
1. De Quervain’s Tenosynovitis
- Affects the thumb side of the wrist
- Involves the abductor pollicis longus and extensor pollicis brevis
- Often caused by repetitive thumb or wrist motion
2. Flexor Tenosynovitis
- Affects the flexor tendons of the fingers
- Can lead to “trigger finger”, where the finger locks in a bent position
- May be associated with diabetes or rheumatoid arthritis
3. Extensor Tenosynovitis
- Involves tendons on the back of the hand or foot
- Often linked to overuse injuries or trauma
Pathophysiology of Tenosynovitis
The synovial sheath produces synovial fluid that lubricates tendon movement. When the sheath becomes inflamed due to irritation or infection, the fluid production may change, and the tendon may catch, swell, or become painful.
Causes and Risk Factors
Repetitive Motion
Repetitive activities such as typing, texting, gripping tools, or sports that strain the tendons can trigger inflammation.
Trauma or Injury
A blow or strain to a tendon area may lead to acute inflammation of the sheath.
Infections
Certain bacterial infections, particularly Staphylococcus aureus, can lead to septic tenosynovitis, requiring urgent care.
Systemic Conditions
- Rheumatoid arthritis
- Gout
- Lupus
- Diabetes mellitus
These systemic inflammatory conditions increase the risk of chronic tenosynovitis.
Symptoms of Tenosynovitis
- Localized pain along the affected tendon
- Swelling and warmth
- Crepitus (a crackling sensation when the tendon moves)
- Restricted range of motion
- Tenderness to touch
- In septic cases: fever, redness, and severe pain
Symptoms typically worsen with activity and improve with rest, especially in non-infectious types.
Diagnosis of Tenosynovitis
Clinical Examination
- Palpation of the affected area reveals pain and swelling
- Specific tests like Finkelstein’s test are used in De Quervain’s diagnosis
Imaging
- Ultrasound: Effective for visualizing fluid accumulation and sheath thickening
- MRI: Useful for detecting chronic or deep-seated inflammation
- X-rays: Rule out underlying joint or bone pathology
Laboratory Tests
In cases of suspected infection or autoimmune disease:
- CBC, CRP, ESR
- Synovial fluid analysis if pus or infection is suspected
Treatment Options for Tenosynovitis
Conservative Treatment
1. Rest and Immobilization
- Use of splints or braces to minimize movement
- Avoid aggravating activities
2. Ice and Anti-Inflammatory Measures
- Cold packs to reduce swelling
- NSAIDs (e.g., ibuprofen, naproxen)
3. Physical Therapy
- Gentle range-of-motion exercises
- Stretching and strengthening of surrounding muscles
4. Corticosteroid Injections
- Injected into the tendon sheath to reduce inflammation
- Particularly effective in De Quervain’s and trigger finger
Surgical Intervention
If conservative therapy fails:
- Tenosynovectomy: Removal of the inflamed sheath
- Trigger release surgery: Cutting of the A1 pulley in trigger finger
Surgery is typically reserved for chronic, unresponsive, or infected cases.
Treatment of Septic Tenosynovitis
- Urgent surgical drainage
- IV antibiotics
- Hospitalization may be required
Prompt intervention is vital to prevent tendon necrosis or joint damage.
Prognosis and Recovery
With early diagnosis and treatment, most tenosynovitis cases resolve without long-term consequences. Recovery duration depends on:
- Severity
- Cause (e.g., infection vs. overuse)
- Patient compliance with therapy
Rehabilitation exercises and ergonomic adjustments play a crucial role in preventing recurrence.
Prevention Strategies
- Ergonomic tools for repetitive tasks
- Frequent breaks during activities like typing
- Proper stretching before physical activity
- Avoiding repetitive strain through smart task design
- Prompt treatment of minor tendon pain
Frequently Asked Questions:
What is the difference between tendonitis and tenosynovitis?
Tendonitis is inflammation of the tendon itself, while tenosynovitis involves inflammation of the sheath surrounding the tendon.
Can tenosynovitis heal on its own?
Mild cases may resolve with rest and conservative care, but chronic or infectious types often need medical treatment.
How long does it take to recover from tenosynovitis?
Recovery varies from a few weeks to several months, depending on severity and treatment adherence.
Is tenosynovitis a form of arthritis?
Not exactly. However, it can be associated with inflammatory arthritis, such as rheumatoid arthritis.
Can I continue to exercise with tenosynovitis?
Low-impact movement may be allowed, but resting the affected area is crucial for healing. Consult a physician or physiotherapist.
Tenosynovitis, while often overlooked, is a significant musculoskeletal condition that can impair daily activities and quality of life. Whether caused by overuse, systemic disease, or infection, early recognition and tailored treatment are key to effective recovery. A comprehensive approach involving clinical evaluation, imaging, conservative therapy, and surgical options when necessary ensures optimal outcomes. Preventive strategies and ergonomic interventions play a pivotal role in reducing recurrence, especially among individuals exposed to repetitive tasks.

