Systemic-onset juvenile idiopathic arthritis (SJIA) is a rare and severe form of juvenile arthritis that primarily affects children under the age of 16. Unlike other types of juvenile idiopathic arthritis (JIA), SJIA is characterized by systemic inflammation, meaning it can affect not only the joints but also other organs and systems of the body. This condition is also referred to as Still’s disease in children and can be particularly challenging to diagnose and manage due to its complex symptoms and multi-organ involvement.
SJIA is an autoimmune disorder where the body’s immune system attacks its own tissues, leading to inflammation. Early diagnosis and appropriate treatment are crucial to preventing long-term damage and improving quality of life for affected children. In this article, we will explore the causes, symptoms, diagnosis, treatment options, and management strategies for systemic-onset juvenile idiopathic arthritis.
Causes of Systemic-Onset Juvenile Idiopathic Arthritis
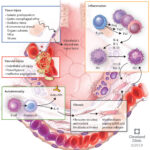
The Role of the Immune System
The exact cause of SJIA remains unclear, but it is believed to involve a combination of genetic and environmental factors. As an autoimmune condition, SJIA occurs when the immune system mistakenly attacks healthy tissues, particularly in the joints and other organs. In systemic-onset JIA, the inflammation is widespread and can affect various parts of the body, including the skin, liver, and heart.
Genetic Predisposition
Research suggests that certain genetic factors may predispose individuals to develop SJIA. Variations in immune-related genes, particularly those related to the regulation of the body’s inflammatory response, are thought to increase susceptibility. The presence of certain HLA (human leukocyte antigen) alleles has been linked to an increased risk of developing SJIA.
Environmental Triggers
Environmental factors, such as viral infections, may also play a role in triggering SJIA in genetically predisposed children. However, no specific environmental triggers have been definitively identified. Infections, especially viral infections, are often considered potential triggers for the onset of disease in children with a genetic predisposition to autoimmunity.
Symptoms of Systemic-Onset Juvenile Idiopathic Arthritis
Classic Features of SJIA
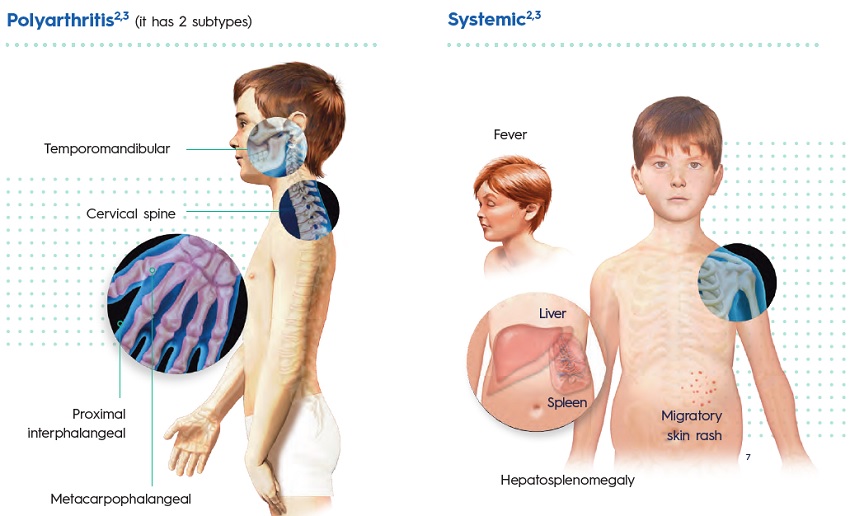
The hallmark feature of systemic-onset JIA is the presence of systemic inflammation, which affects not only the joints but also various other organs in the body. The most common symptoms include:
- High Fever: One of the most distinctive symptoms of SJIA is a high, spiking fever that typically occurs once or twice a day, often in the evening or late afternoon. The fever is often accompanied by chills and may last for weeks or months.
- Salmon-Colored Rash: A unique, salmon-colored rash often accompanies the fever. This rash usually appears on the trunk and limbs and may come and go, often worsening with fever spikes.
- Joint Inflammation: Joint swelling, pain, and stiffness are common in SJIA. The joints most affected are typically large joints such as the knees, hips, and wrists, but it can also affect smaller joints. The joint inflammation can lead to significant discomfort and disability.
Other Systemic Symptoms
In addition to the primary symptoms, SJIA can also cause other systemic manifestations:
- Enlarged Lymph Nodes: Swelling of the lymph nodes, especially in the neck and armpit, is often seen in children with SJIA.
- Liver and Spleen Enlargement: Children with SJIA may develop hepatosplenomegaly, or enlargement of the liver and spleen, as a result of systemic inflammation.
- Anemia: Due to chronic inflammation, children with SJIA may develop anemia, leading to fatigue and weakness.
- Growth Delay: Chronic inflammation and the use of corticosteroid medications can interfere with normal growth in children with SJIA.
Diagnosis of Systemic-Onset Juvenile Idiopathic Arthritis
Clinical Evaluation and History
The diagnosis of SJIA is based on a combination of clinical signs and symptoms, as well as exclusion of other conditions. A detailed medical history, including the presence of fever, rash, and joint symptoms, is essential. The pattern of fever spikes and the characteristic salmon-colored rash are key diagnostic clues.
Laboratory Tests
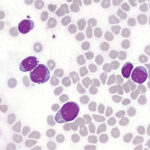
Several laboratory tests are used to confirm the diagnosis and rule out other conditions:
- Blood Tests: Elevated levels of C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), which indicate systemic inflammation, are common in SJIA. Additionally, blood tests often show anemia and thrombocytosis (increased platelet count).
- Antinuclear Antibody (ANA) and Rheumatoid Factor (RF): Unlike other forms of juvenile arthritis, SJIA is typically negative for ANA and RF, which helps distinguish it from other autoimmune diseases like juvenile rheumatoid arthritis (JRA).
- Joint Imaging: X-rays or ultrasounds may be used to evaluate joint damage and inflammation, although imaging findings are not typically as prominent in the early stages of SJIA.
Exclusion of Other Conditions
The diagnosis of SJIA is one of exclusion, meaning other possible causes of systemic inflammation, such as infections or malignancies, must be ruled out before confirming the diagnosis. SJIA is typically diagnosed after other potential causes of fever and joint symptoms have been considered.
Treatment of Systemic-Onset Juvenile Idiopathic Arthritis
Medications for Systemic-Onset JIA
The treatment of SJIA focuses on reducing inflammation, managing symptoms, and preventing long-term damage to the joints and organs. The primary treatments include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs such as ibuprofen are often used to reduce pain and inflammation, particularly in the early stages of the disease.
- Corticosteroids: High-dose corticosteroids (e.g., prednisone) are frequently used to manage acute inflammation, particularly during disease flares. Long-term use, however, is avoided due to the potential for side effects such as growth retardation and osteoporosis.
- Disease-Modifying Antirheumatic Drugs (DMARDs): In cases where NSAIDs and corticosteroids are insufficient, DMARDs like methotrexate may be prescribed to modify the disease’s course and prevent joint damage.
- Biologic Agents: Biologic drugs targeting specific components of the immune system, such as interleukin-1 (IL-1) inhibitors (e.g., anakinra) and interleukin-6 (IL-6) inhibitors (e.g., tocilizumab), have shown significant efficacy in treating SJIA, especially in cases that do not respond to conventional medications.
Symptomatic Treatment
In addition to the above medications, symptomatic treatment for joint pain and stiffness includes physical therapy, joint protection techniques, and the use of assistive devices when necessary. Occupational therapy can help children maintain independence in daily activities despite the functional limitations caused by arthritis.
Prognosis and Long-Term Management
The prognosis of systemic-onset juvenile idiopathic arthritis varies depending on the severity of the disease and the effectiveness of treatment. With early diagnosis and appropriate therapy, many children with SJIA can achieve remission or minimal disease activity. However, some may experience chronic joint damage and complications, such as growth problems and developmental delays.
Regular Monitoring and Follow-Up
Ongoing monitoring of disease activity, including regular blood tests, joint assessments, and imaging studies, is essential for managing SJIA effectively. Early identification of complications such as uveitis (inflammation of the eye) or pulmonary involvement can significantly improve long-term outcomes.
Emotional and Social Support
Children with SJIA may face significant emotional and social challenges, particularly if the disease causes physical limitations or affects their ability to participate in normal childhood activities. Psychosocial support, including counseling and peer support groups, can help children and their families cope with the emotional burden of the disease.
Systemic-onset juvenile idiopathic arthritis is a severe and complex disease that requires early diagnosis and comprehensive management to prevent long-term damage and improve quality of life. With advancements in treatment, including biologic agents and improved supportive care, the outlook for children with SJIA has significantly improved. However, ongoing monitoring and tailored treatment strategies remain essential for managing this chronic inflammatory condition effectively. Through a multidisciplinary approach, children with SJIA can lead healthier, more active lives despite the challenges posed by this autoimmune disease.