Systemic cryptococcosis, primarily caused by Cryptococcus neoformans and Cryptococcus gattii, represents a severe fungal infection that often manifests as cryptococcal meningoencephalitis. This life-threatening condition frequently affects immunocompromised individuals, notably those with advanced HIV/AIDS, solid organ transplants, or hematologic malignancies.
While antifungal agents remain the cornerstone of therapy, adjunctive strategies are crucial to improve survival, manage complications such as raised intracranial pressure (ICP), and enhance antifungal drug efficacy. High mortality rates, especially in low-resource settings, necessitate a holistic, multi-pronged treatment model.
Antifungal Treatment Backbone: Induction, Consolidation, and Maintenance
Induction Therapy
- Amphotericin B deoxycholate or liposomal formulations (L-AmB)
- Flucytosine (5-FC)
- Duration: 2 weeks (extended in severe cases)
Combination of Amphotericin B and Flucytosine has demonstrated the highest early fungicidal activity, reducing cerebrospinal fluid (CSF) fungal burden and improving patient outcomes.
Consolidation Phase
- High-dose Fluconazole (800 mg/day)
- Duration: At least 8 weeks following culture clearance
Maintenance Therapy
- Fluconazole (200 mg/day)
- Duration: Minimum 12 months, or until immune reconstitution (CD4 > 100 cells/μL for 3+ months with virologic suppression)
Adjunctive Therapy in Systemic Cryptococcosis: Mechanisms and Clinical Application
Adjunctive therapies enhance the effectiveness of antifungal treatment, manage systemic complications, and tailor interventions to specific patient populations.
Intracranial Pressure Management: Critical Adjunct in Cryptococcal Meningitis
Pathophysiology and Prevalence
Increased ICP occurs in over 60% of cryptococcal meningitis patients due to impaired CSF absorption and fungal polysaccharide obstruction. Elevated ICP is a leading cause of morbidity and mortality.
Therapeutic Measures
- Serial lumbar punctures: Gold standard for symptomatic relief and pressure control (>25 cm H₂O)
- External ventricular drain (EVD): Reserved for refractory cases
- Avoidance of corticosteroids: Shown to increase mortality in the CryptoDex trial
Aggressive control of ICP is directly associated with reduced neurological sequelae and improved survival.
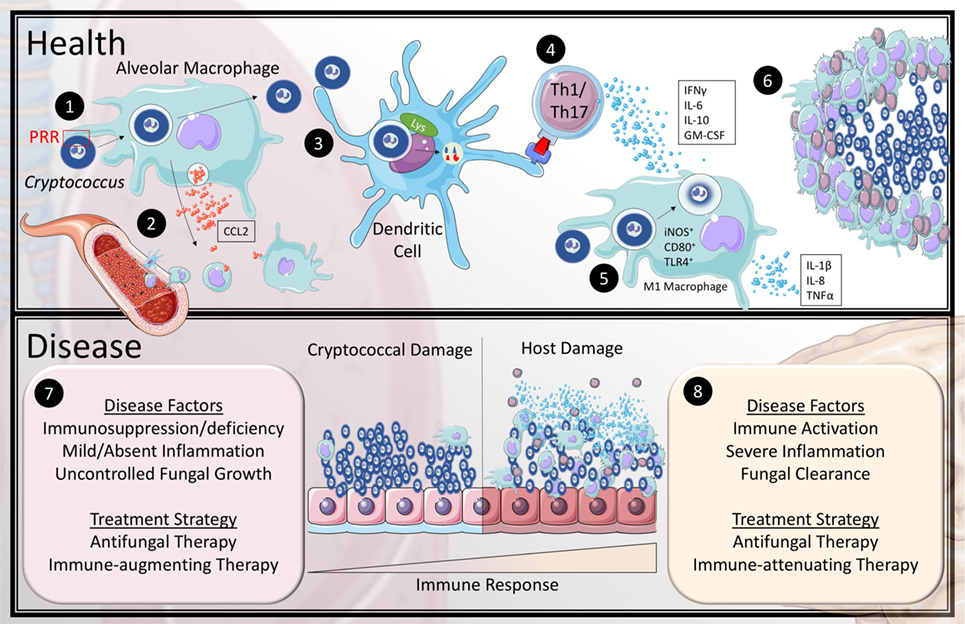
Immunomodulatory Adjuncts: Balancing Host Response
Antiretroviral Therapy (ART) Timing in HIV
- Initiate 4–6 weeks after antifungal therapy start to avoid immune reconstitution inflammatory syndrome (IRIS)
- Early ART initiation (<2 weeks) linked to increased mortality due to unmasking or paradoxical IRIS
Interferon-Gamma (IFN-γ) Therapy
- Enhances macrophage activation and antifungal clearance
- Randomized trials demonstrate improved early fungicidal activity when used adjunctively with antifungals
- Regimen: 100–200 μg subcutaneously, three times weekly for 2–3 weeks
Adjunctive Diagnostics and Monitoring
Fungal Burden Assessment
- Cryptococcal antigen (CrAg) titers in CSF and serum
- Quantitative cultures: Useful for monitoring clearance
Imaging
- MRI/CT scan of the brain: Essential for identifying cryptococcomas, hydrocephalus, or ischemic changes
Laboratory Parameters
- Monitor for renal toxicity (especially with Amphotericin B)
- Regular hematologic panels due to bone marrow suppression from flucytosine
Novel and Investigational Adjunctive Therapies
Sertraline
- Antidepressant with in vitro antifungal activity
- Early trials showed promise, but recent Phase III trials (ASTRO-CM) showed no survival benefit
- Currently not recommended as a standard adjunct
Repurposed Drugs and Immunotherapies
- Tamoxifen, calcineurin inhibitors, and monoclonal antibodies under investigation
- Cryptococcal vaccines: Still in preclinical phases but may serve future adjunctive roles
Adjunctive Care in Non-HIV Populations
Organ Transplant Recipients
- Require reduction of immunosuppression during active infection
- Liposomal Amphotericin B preferred to minimize nephrotoxicity
Cryptococcus gattii Infection
- More likely to form cryptococcomas
- Often affects immunocompetent individuals
- Requires extended antifungal therapy and potential neurosurgical interventions
Key Recommendations for Clinical Practice
| Intervention | Recommendation | Clinical Justification |
|---|---|---|
| Amphotericin B + Flucytosine | First-line induction regimen | Best early fungicidal activity |
| Serial lumbar punctures | ICP ≥ 25 cm H₂O or symptomatic | Reduces morbidity from raised ICP |
| ART deferral in HIV | Initiate at 4–6 weeks | Reduces IRIS-related mortality |
| IFN-γ adjunctive therapy | Consider in persistent high burden cases | Enhances immune clearance |
| Avoid corticosteroids | Routine use discouraged | Associated with higher mortality |
| Regular CrAg and fungal culture | Monitor therapeutic response | Guides transition between therapy phases |
Frequently Asked Questions:
Q1. What is the most effective induction treatment for systemic cryptococcosis?
Amphotericin B combined with flucytosine offers the highest efficacy and is the current gold standard.
Q2. Why is management of intracranial pressure important in cryptococcal meningitis?
Because uncontrolled ICP is a leading cause of death; managing it reduces neurological damage and improves survival.
Q3. Can corticosteroids be used as adjuncts in systemic cryptococcosis?
No. Corticosteroids are contraindicated due to increased mortality, except in rare cases of confirmed IRIS.
Q4. Is interferon-gamma therapy widely used in cryptococcal infection?
It is used selectively in high-burden cases or where immune response needs augmentation, typically in clinical trial settings.
Q5. How soon should ART be started in HIV patients with cryptococcosis?
ART should be initiated 4–6 weeks after the start of antifungal therapy to minimize IRIS and mortality.

