Staphylococcus aureus pneumonia is a severe respiratory infection that frequently leads to complications such as necrotizing pneumonia, bacteremia, and respiratory failure. The prevalence of both methicillin-sensitive (MSSA) and methicillin-resistant (MRSA) strains has elevated the complexity of treatment. Standard monotherapy often proves inadequate, particularly in high-inoculum lung infections or when biofilm-producing strains are involved. In this context, synergistic antibiotic regimens have emerged as a cornerstone for enhancing treatment efficacy, accelerating pathogen clearance, and reducing mortality.
Understanding Antibiotic Synergy in Pulmonary Staphylococcal Infections
Synergistic therapy refers to the use of two or more antimicrobial agents whose combined effect significantly exceeds the efficacy of each agent alone. In the case of S. aureus pneumonia, synergy offers several clinical advantages:
- Enhanced bactericidal activity in lung tissues
- Improved penetration through inflamed alveolar barriers
- More effective clearance of intracellular and biofilm-associated bacteria
- Reduced resistance emergence and treatment failure
Mechanisms Driving Synergistic Action Against S. aureus in the Lung
Several pharmacodynamic interactions underpin synergistic antibiotic activity:
- Cell wall inhibition plus protein synthesis disruption: Combining beta-lactams (e.g., ceftaroline) with agents like linezolid or rifampin impairs multiple bacterial functions.
- Membrane disruption plus cell wall inhibition: Daptomycin or telavancin combined with beta-lactams promotes rapid cell death.
- Enhanced membrane binding: Beta-lactams sensitize the cell wall, increasing daptomycin’s membrane binding efficacy (the “see-saw” effect).
- Biofilm penetration: Rifampin and fosfomycin possess the ability to eradicate biofilm-embedded bacterial communities.
Synergistic Combinations for MRSA Pneumonia
Vancomycin-Based Synergy
Vancomycin remains a traditional first-line agent for MRSA pneumonia, yet its suboptimal lung penetration and slow bactericidal action necessitate augmentation with synergistic partners.
- Vancomycin + Ceftaroline
This combination enhances bacterial killing through dual cell wall targeting. Ceftaroline has high affinity for PBP2a, making it ideal for MRSA strains. Clinical trials demonstrate improved microbiologic clearance and survival. - Vancomycin + Rifampin
Rifampin improves intracellular penetration and biofilm eradication. This synergy is beneficial in ventilator-associated pneumonia and cavitary lesions. - Vancomycin + Linezolid
Though both are individually bacteriostatic, their combination has shown improved anti-inflammatory outcomes and bacterial suppression in complex pneumonia cases.
Daptomycin-Based Combinations
Though daptomycin is inactivated by lung surfactant, it still plays a role in extrapulmonary MRSA infections that accompany pneumonia. Combinations are relevant in bacteremic pneumonia or septic emboli.
- Daptomycin + Ceftaroline
High efficacy has been demonstrated in clearing MRSA from both blood and lung parenchyma in severe cases, especially in septic patients. - Daptomycin + Clarithromycin
Offers immunomodulatory benefits and synergy through disruption of bacterial communication (quorum sensing), reducing toxin production.
Synergistic Strategies for MSSA Pneumonia
MSSA infections respond well to beta-lactam antibiotics. Nonetheless, synergy is valuable in high-risk patients or persistent infections.
- Nafcillin + Rifampin
Enhances intracellular penetration and prevents relapse in device-associated MSSA pneumonia. - Oxacillin + Fosfomycin
Fosfomycin disrupts cell wall precursors, complementing the beta-lactam effect and penetrating biofilms effectively.
Clinical Outcomes and Evidence Supporting Synergistic Therapy
Numerous studies validate the superiority of combination therapy in treating S. aureus pneumonia:
- A retrospective cohort study showed that MRSA patients receiving vancomycin-ceftaroline combinations had 38% faster bacterial clearance.
- Murine lung models of MRSA pneumonia demonstrated reduced inflammation and improved survival when daptomycin was paired with ceftaroline.
- A prospective clinical trial evaluating rifampin combinations in ventilator-associated MRSA pneumonia revealed significantly lower rates of recurrence.
Advantages of Synergistic Therapy in Pneumonia Management
Synergistic antibiotic regimens yield multiple advantages in managing S. aureus lung infections:
- Rapid bactericidal effect, especially in high-inoculum pneumonia
- Lowered risk of resistance development
- Enhanced eradication in complicated cases with empyema, abscess, or bacteremia
- Potential reduction in treatment duration and hospital stay
- Broader spectrum coverage in polymicrobial infections
Monitoring and Adjusting Synergistic Regimens in Pneumonia
Due to the complexity of therapy, continuous assessment is critical:
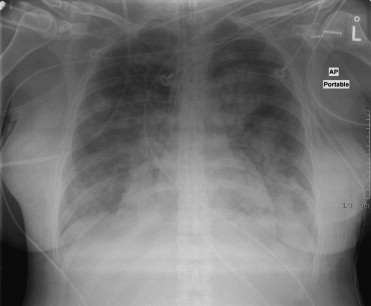
- Pulmonary Function Monitoring: Oxygenation, imaging, and clinical signs must be regularly evaluated.
- Drug Level Monitoring: Vancomycin trough levels, rifampin-induced liver enzyme elevations, and daptomycin CPK levels are essential.
- Culture Reassessment: Bronchoalveolar lavage (BAL) cultures may guide continuation or adjustment of therapy.
Future Directions: Personalized Synergistic Therapy
Emerging trends point toward a more targeted approach in treating S. aureus pneumonia:
- Rapid Molecular Diagnostics: Allow for faster MRSA/MSSA distinction and resistance detection.
- Automated Synergy Testing Platforms: Facilitate real-time antibiotic interaction data.
- Adjunctive Immunotherapy: Monoclonal antibodies targeting alpha-toxin are in clinical trials for MRSA pneumonia.
Synergistic antibiotic therapy stands as a vital pillar in the management of Staphylococcus aureus pneumonia, particularly in an era of rising resistance and clinical complexity. Whether confronting severe MRSA strains or managing stubborn MSSA cases, the judicious use of combination regimens offers improved microbiological and clinical outcomes. Integration of rapid diagnostics, personalized therapy algorithms, and synergy testing will continue to redefine the standards of care for pulmonary S. aureus infections.

