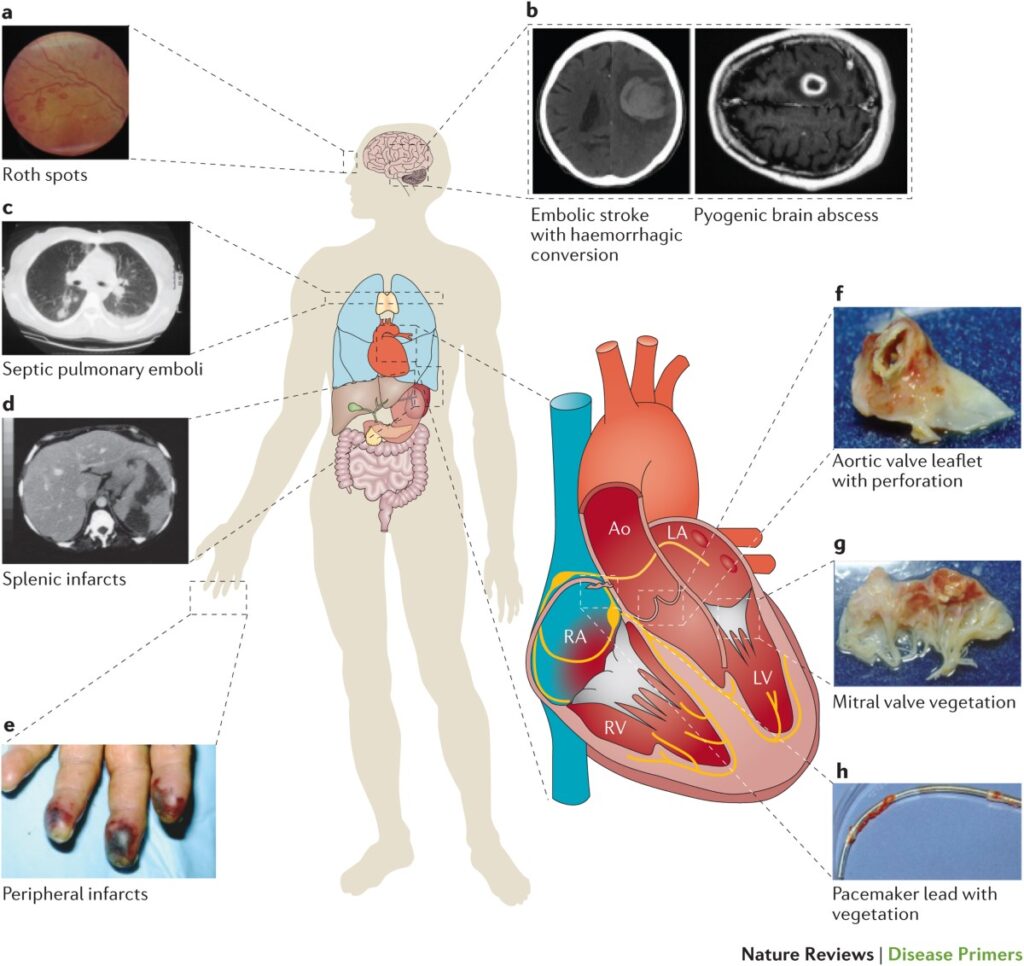
Staphylococcal endocarditis, primarily caused by Staphylococcus aureus and Staphylococcus epidermidis, remains one of the most severe and life-threatening infective endocarditis (IE) variants. With rising methicillin-resistant strains (MRSA) and treatment-refractory infections involving prosthetic valves or implantable devices, optimal antibiotic synergy is paramount for therapeutic success.
Infective endocarditis results from the colonization of cardiac valves by bacteria, often following bacteremia. S. aureus is distinguished by its aggressive tissue invasion, biofilm formation, and toxin production. These traits necessitate a treatment regimen beyond monotherapy, especially for persistent or prosthetic valve infections.
Clinical Significance of Synergy in Staphylococcal Endocarditis
Antibiotic synergy refers to the enhanced bactericidal activity observed when two or more agents are combined, often targeting different bacterial processes. In staphylococcal endocarditis, synergy is crucial due to:
- Dense vegetations reducing antibiotic penetration
- Persistent intracellular infections
- Biofilm-associated resistance on prosthetic materials
- High bacterial inoculum requiring bactericidal activity
Combination regimens, especially those incorporating aminoglycosides, rifampin, or newer lipopeptides, have demonstrated superior efficacy in these settings.
Mechanisms of Synergistic Antibiotic Combinations
Effective synergy in staphylococcal endocarditis often involves a multifaceted attack on bacterial physiology:
- Cell wall synthesis inhibitors (e.g., beta-lactams, vancomycin) weaken the structural integrity of the cell.
- Protein synthesis inhibitors (e.g., gentamicin, linezolid) prevent bacterial replication and toxin production.
- RNA synthesis inhibitors (e.g., rifampin) penetrate biofilms and target dormant bacteria.
This layered approach enhances bacterial killing, prevents resistance selection, and eradicates persistent bacterial populations.
Key Synergistic Combinations in Clinical Practice
1. Nafcillin or Oxacillin + Gentamicin (MSSA)
- Target: Methicillin-sensitive S. aureus (MSSA)
- Mechanism: Beta-lactam disrupts cell wall, allowing gentamicin enhanced intracellular penetration
- Use Case: Short-term synergy for severe native valve endocarditis
- Limitations: Risk of nephrotoxicity restricts duration to ≤5 days
2. Vancomycin + Rifampin + Gentamicin (MRSA Prosthetic Valve Endocarditis)
- Target: Methicillin-resistant S. aureus in prosthetic material
- Mechanism: Vancomycin disrupts wall synthesis; rifampin penetrates biofilms; gentamicin boosts killing
- Indication: First-line for MRSA prosthetic valve endocarditis per AHA/IDSA guidelines
- Note: Rifampin must never be used as monotherapy due to rapid resistance development
3. Daptomycin + Ceftaroline
- Target: Persistent MRSA or vancomycin non-responders
- Mechanism: Daptomycin targets membrane potential; ceftaroline restores daptomycin binding sites
- Evidence: Demonstrated synergy in salvage therapy for persistent bacteremia
- Benefit: Lower MICs, reduced mortality in case series and in vitro models
4. Linezolid + Rifampin
- Target: Drug-resistant coagulase-negative staphylococci and prosthetic device infections
- Mechanism: Linezolid halts protein synthesis; rifampin aids biofilm penetration
- Caution: Monitor for thrombocytopenia with long-term linezolid use
Role of Synergy in Special Populations
Prosthetic Valve Endocarditis (PVE)
Synergy is critical in PVE due to the protective niche created by biofilms on prosthetic materials. Rifampin-containing regimens remain standard, supported by decades of clinical data.
Persistent Bacteremia
When bacteremia persists beyond 72 hours on appropriate therapy, combination regimens such as daptomycin-ceftaroline or vancomycin-gentamicin may be employed to accelerate clearance.
Pediatric Considerations
In children, synergy is used cautiously due to higher toxicity risks. Nevertheless, gentamicin or rifampin may be considered for severe cases, under close monitoring.
In Vitro and Clinical Evidence Supporting Synergy
- Time-kill assays confirm synergistic bactericidal effects with combinations like vancomycin-rifampin-gentamicin
- Animal models of endocarditis show improved survival with synergistic regimens
- Clinical series highlight success in refractory MRSA with daptomycin plus ceftaroline
- Meta-analyses suggest reduced mortality in persistent MRSA bacteremia with combination therapy
Monitoring and Toxicity Considerations
Aminoglycosides
- Monitor renal function and drug levels (especially peak and trough)
- Limit duration to reduce ototoxicity and nephrotoxicity
Rifampin
- Monitor liver enzymes
- Watch for drug interactions via CYP450 induction
Daptomycin
- Monitor creatine phosphokinase (CPK) weekly
- Discontinue if muscle toxicity signs develop
The Future of Synergistic Therapy in Endocarditis
Advancements in molecular diagnostics and susceptibility testing allow for real-time identification of optimal combinations. Research is ongoing into:
- Phage-antibiotic synergy
- Monoclonal antibody adjuncts
- Nanoparticle-based antibiotic delivery
- AI-assisted synergy prediction tools
Personalized antimicrobial therapy, guided by synergy testing, is expected to become standard in the management of complex staphylococcal endocarditis.
Synergistic antibiotic therapy is a cornerstone in the successful management of staphylococcal endocarditis, especially in the context of MRSA, prosthetic material, and persistent bacteremia. By combining agents with complementary mechanisms, we achieve superior bactericidal activity, resistance mitigation, and improved patient outcomes. Tailoring synergy based on pathogen profile, clinical presentation, and patient tolerance is essential for optimizing care.