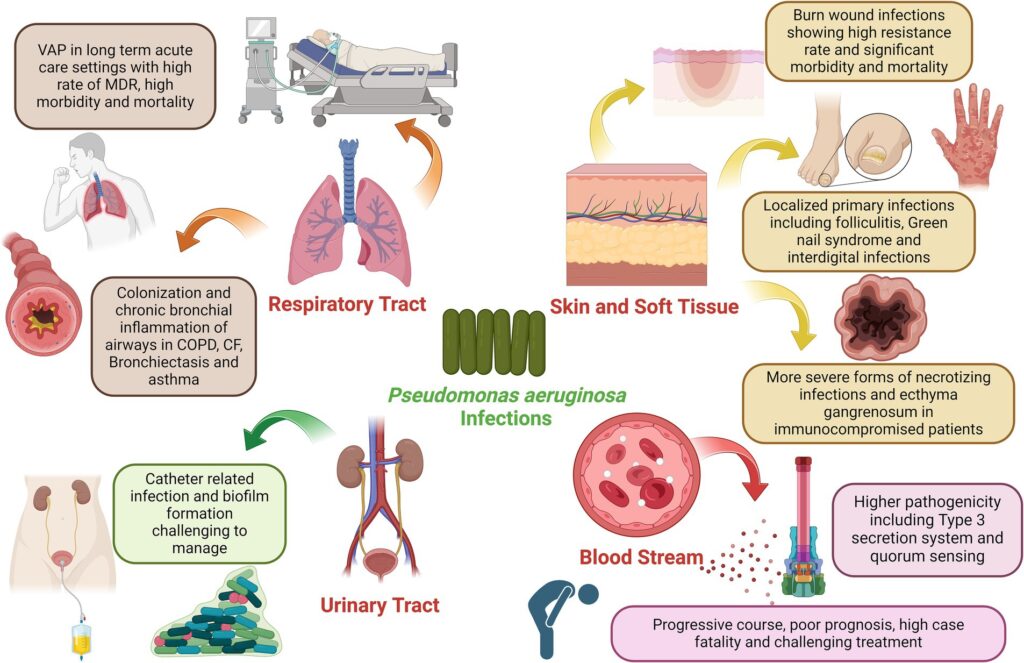
Pseudomonas aeruginosa is a gram-negative, opportunistic pathogen known for causing severe skin and skin structure infections (SSSIs), especially in immunocompromised individuals and patients with burns, wounds, or surgical incisions. These infections are particularly challenging due to the organism’s innate resistance mechanisms and biofilm-forming capabilities.
SSSIs caused by P. aeruginosa demand rapid and targeted intervention, as the pathogen is notorious for multidrug resistance (MDR) and its ability to evade monotherapy. In recent years, research has increasingly focused on antibiotic synergy to enhance clinical outcomes and combat resistance development.
Pathophysiology and Clinical Presentation
In SSSIs, P. aeruginosa typically enters through breaches in the dermal barrier. Once established, it triggers an aggressive inflammatory response, characterized by tissue necrosis, edema, and purulent discharge. Common presentations include:
- Burn wound infections
- Post-surgical abscesses
- Diabetic foot ulcers
- Chronic wounds and ulcers
- Folliculitis and ecthyma gangrenosum (in severe cases)
Its virulence factors, such as exotoxins, elastases, and quorum-sensing molecules, enable rapid tissue invasion and immune evasion.
Challenges in Treating Pseudomonas aeruginosa SSSIs
Multidrug Resistance (MDR)
MDR P. aeruginosa strains exhibit resistance through multiple mechanisms, including:
- Efflux pumps (e.g., MexAB-OprM)
- Beta-lactamase production
- Altered porin channels
- Biofilm formation reducing antibiotic penetration
Monotherapy Limitations
Monotherapy, even with potent antipseudomonal agents like piperacillin-tazobactam or meropenem, often fails due to rapid adaptation and resistance emergence. As such, synergistic antibiotic combinations are increasingly employed.
Mechanisms and Benefits of Antibiotic Synergy
Synergy occurs when the combined effect of two or more antibiotics exceeds the additive effect of individual agents. Synergistic mechanisms include:
- Cell wall disruption + protein synthesis inhibition: Enhances antibiotic entry and bacterial killing.
- Beta-lactam + aminoglycoside: Beta-lactams weaken the cell wall, facilitating aminoglycoside penetration.
- Fluoroquinolone + polymyxin: Targets both DNA synthesis and membrane integrity.
This approach reduces bacterial load more efficiently, lowers resistance potential, and may allow dose reduction to minimize toxicity.
Synergistic Antibiotic Combinations for Pseudomonas aeruginosa
1. Beta-Lactam + Aminoglycoside
- Common Pairings: Piperacillin-tazobactam + amikacin or gentamicin
- Advantages: Effective for deep-seated infections and bacteremia associated with SSSIs
- Caveats: Nephrotoxicity risk; requires renal function monitoring
2. Carbapenem + Polymyxin B or Colistin
- Mechanism: Dual attack on the cell wall and membrane
- Usage: Reserved for extensively drug-resistant (XDR) strains
- Concerns: High nephrotoxicity; requires therapeutic drug monitoring
3. Fluoroquinolone + Beta-Lactam
- Example: Ceftazidime + ciprofloxacin
- Evidence: In vitro and clinical studies show enhanced killing and biofilm suppression
- Ideal For: Outpatient regimens or step-down therapy
4. Ceftolozane-Tazobactam + Fosfomycin
- Utility: Novel combination with promising synergy in MDR isolates
- Benefit: Fosfomycin’s unique mechanism complements ceftolozane’s strong activity
5. Dual Beta-Lactam Therapy
- Experimental Approach: Aztreonam + ceftazidime-avibactam for metallo-beta-lactamase producers
- Rationale: Broader coverage and beta-lactamase inhibition
Clinical Evidence Supporting Synergy in SSTI Management
Multiple studies support combination therapy for enhanced clinical and microbiological outcomes in P. aeruginosa SSTIs:
- Meta-analyses demonstrate higher success rates in MDR infections with dual therapy compared to monotherapy.
- In vitro time-kill studies reveal significant bacterial suppression with beta-lactam/aminoglycoside or beta-lactam/fluoroquinolone pairings.
- Clinical case series highlight rapid wound healing and reduced hospitalization duration when synergy is employed.
Local Wound Management and Adjunctive Therapy
Effective SSSI treatment is not limited to systemic antibiotics. Local wound care is pivotal:
- Debridement: Removal of necrotic tissue enhances penetration and efficacy
- Topical Agents: Silver sulfadiazine, acetic acid, or polymyxin-based dressings
- Negative Pressure Wound Therapy (NPWT): Promotes granulation and fluid removal
- Adjunctive Immunotherapy: Investigational use of phage therapy or monoclonal antibodies
Antibiotic Stewardship and Resistance Prevention
Optimizing synergy also supports antimicrobial stewardship by:
- Avoiding unnecessary broad-spectrum monotherapy
- Limiting resistance by targeting specific mechanisms
- Allowing de-escalation based on culture sensitivity
De-escalation strategies must be aligned with local antibiograms and resistance trends.
The synergistic use of antibiotics in treating skin and skin structure infections caused by Pseudomonas aeruginosa offers a robust, evidence-backed approach to overcome drug resistance, improve clinical outcomes, and minimize adverse effects. By combining agents with complementary mechanisms, clinicians can achieve higher bacterial eradication rates and reduce the burden of chronic and complicated infections.