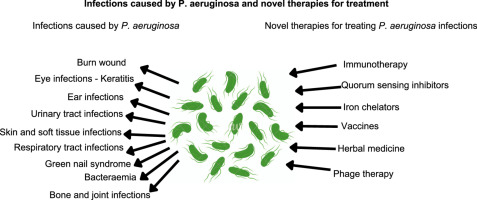
Pseudomonas aeruginosa is a leading cause of healthcare-associated bloodstream infections (BSIs), especially in immunocompromised or critically ill patients. Its ability to survive in diverse environments, along with its extensive resistance mechanisms, makes septicemia caused by this organism particularly difficult to treat.
Mortality rates remain alarmingly high, with figures ranging from 30% to over 60% in septic shock. Early, aggressive, and precisely tailored combination therapy is critical in managing these life-threatening infections.
The Rationale Behind Antibiotic Synergy in Septicemia
Synergy refers to the cooperative effect of combining two or more antimicrobials to produce a greater bacterial kill rate than each agent alone. This approach is especially effective against P. aeruginosa, a pathogen that exhibits:
- Efflux-mediated resistance
- Enzymatic β-lactam degradation
- Biofilm-associated protection
- Porin channel mutations
In the bloodstream, where rapid bacterial multiplication and toxin release can cause systemic collapse, synergistic therapy maximizes early bacterial clearance and prevents resistance emergence.
Key Antibiotic Combinations for Synergistic Activity
1. β-Lactam and Aminoglycoside Combinations
Piperacillin-Tazobactam + Amikacin
This combination is one of the most validated regimens for empirical therapy in suspected P. aeruginosa bacteremia. The β-lactam compromises cell wall integrity, enhancing aminoglycoside penetration and protein synthesis inhibition.
Cefepime + Gentamicin
Demonstrates significant time-kill synergy in bloodstream isolates. Cefepime has high stability against AmpC β-lactamases, making it a strong partner in dual therapy.
2. β-Lactam and Fluoroquinolone Combinations
Ceftazidime + Ciprofloxacin
Ceftazidime disrupts the outer membrane while ciprofloxacin targets DNA gyrase and topoisomerase IV. This combination achieves rapid bactericidal activity in bloodstream models.
Meropenem + Levofloxacin
Recommended in neutropenic and ICU patients due to its potent action against both replicating and intracellular P. aeruginosa.
3. Colistin-Based Synergistic Therapy
Colistin + Meropenem
Colistin’s membrane-permeabilizing effect restores susceptibility to carbapenems in resistant isolates. This duo is essential in XDR P. aeruginosa septicemia where options are limited.
Colistin + Rifampicin
Rifampicin enhances intracellular killing, and when used with colistin, it penetrates difficult-to-treat niches like intravascular devices or endothelial reservoirs.
4. Newer Agents and Synergistic Combinations
Ceftolozane-Tazobactam + Amikacin
Offers potent synergy against ESBL- and AmpC-producing strains in BSI, with enhanced time-dependent and concentration-dependent killing.
Fosfomycin + Piperacillin-Tazobactam
Fosfomycin’s unique mechanism bypasses traditional resistance channels, and when paired with β-lactams, disrupts early bacterial cell wall synthesis and metabolism.
In-Vitro and Clinical Evidence of Synergistic Effects
Studies using time-kill assays, checkerboard titration, and hollow-fiber infection models consistently demonstrate:
- Greater than 2-log bacterial reduction within 6–8 hours post-treatment
- Suppressed emergence of resistant subpopulations
- Enhanced pharmacokinetic/pharmacodynamic (PK/PD) outcomes in serum simulations
Clinical trials and retrospective cohort analyses show that patients receiving combination therapy within 24 hours of septicemia onset have significantly reduced mortality compared to monotherapy.
Tailoring Synergy to Clinical Context
Empirical vs. Targeted Therapy
- Empirical therapy should begin with broad-spectrum dual antibiotics in high-risk patients, particularly those with recent hospital exposure, prior antibiotic use, or immunosuppression.
- Targeted therapy should be refined within 48–72 hours based on blood culture and sensitivity results, optimizing synergy while minimizing toxicity.
Risk Stratification for Synergistic Use
| Risk Factor | Recommendation |
|---|---|
| Septic shock | Initiate synergistic dual therapy |
| Neutropenia | Include aminoglycoside or fluoroquinolone |
| Central line-associated BSI | Consider rifampicin for biofilm synergy |
| Prior colonization with MDR strains | Use colistin-based synergistic regimens |
Pharmacodynamic Optimization
To maximize the benefits of synergy:
- Use extended or continuous β-lactam infusions to maintain time-above-MIC
- Front-load aminoglycosides with once-daily dosing for peak/MIC efficacy
- Apply therapeutic drug monitoring (TDM) for colistin and aminoglycosides to avoid nephrotoxicity
Limitations and Considerations
While synergy improves bactericidal action, it must be balanced with:
- Nephrotoxicity risks from aminoglycosides and colistin
- Emergence of resistance during suboptimal dosing
- Drug-drug interactions, particularly in polypharmacy settings
Close monitoring, de-escalation after microbiological confirmation, and adherence to PK/PD principles are essential to avoid adverse outcomes.
Future Prospects in Synergistic Management
Phage-Antibiotic Synergy in Bacteremia
Combining bacteriophages with colistin or carbapenems enhances killing of biofilm-embedded and bloodstream P. aeruginosa, especially in salvage therapy.
Intravascular Device Lock Therapy
Use of synergistic agents in catheter lock solutions (e.g., gentamicin + ethanol) shows promise in preventing and treating line-associated septicemia.
AI-Guided Regimen Selection
Emerging platforms use AI to predict optimal synergistic combinations based on genetic and resistance profiles, aiding real-time clinical decision-making.
Synergistic antibiotic therapy offers a crucial edge in treating Pseudomonas aeruginosa septicemia, particularly in high-risk, drug-resistant scenarios. Precision in choosing the right combinations, timing, and dosing strategies ensures maximal efficacy and improved survival. Continued research and personalized synergy-based protocols are key to addressing the evolving challenge of resistant bloodstream infections.