Pseudomonas aeruginosa meningitis is a rare but life-threatening infection of the central nervous system (CNS), typically associated with neurosurgical procedures, external ventricular drains (EVD), or head trauma. Its management poses a significant clinical challenge due to the organism’s multidrug resistance mechanisms, poor CNS drug penetration, and biofilm-forming capability on intracranial devices.
Pathogenesis and Clinical Presentation
Meningitis caused by P. aeruginosa is often nosocomial and associated with:
- Neurosurgical interventions (e.g., craniotomy, shunt placement)
- Open head trauma with cerebrospinal fluid (CSF) leaks
- Immunocompromised states
- Use of intraventricular catheters
Clinical signs include:
- Fever, altered mental status, photophobia, nuchal rigidity
- Elevated CSF leukocyte count, decreased glucose, and elevated protein
- CSF culture positive for P. aeruginosa
Antimicrobial Resistance and the Need for Synergistic Therapy
P. aeruginosa demonstrates resistance via:
- Efflux pumps (e.g., MexAB-OprM)
- AmpC β-lactamases
- Loss of OprD porin channel (conferring carbapenem resistance)
- Biofilm formation on CNS shunts and catheters
As monotherapy often fails due to these resistance mechanisms, synergistic antibiotic combinations are required to:
- Enhance bactericidal activity
- Ensure therapeutic CNS concentrations
- Overcome the blood-brain barrier (BBB) and biofilm-related protection
Ideal Antibiotic Combinations for Pseudomonas aeruginosa Meningitis
1. Cefepime or Ceftazidime Plus Aminoglycoside
- Cefepime + Amikacin or Ceftazidime + Tobramycin offers synergistic killing.
- Both β-lactams achieve measurable CSF levels, particularly when meninges are inflamed.
- Aminoglycosides have poor BBB penetration systemically; intrathecal/intraventricular administration is often required.
2. Meropenem Plus Colistin
- Recommended for carbapenem-resistant strains.
- Meropenem penetrates CSF efficiently; colistin may be delivered intraventricularly due to limited systemic CNS availability.
- Synergy disrupts bacterial membranes and inhibits cell wall synthesis concurrently.
3. Ceftolozane-Tazobactam Plus Fosfomycin
- Effective against MDR strains with extended resistance patterns.
- Fosfomycin improves penetration through biofilms and increases β-lactam efficacy.
4. Aztreonam Plus Avibactam
- Considered in metallo-β-lactamase (MBL)-producing isolates.
- Aztreonam offers Gram-negative coverage; avibactam restores aztreonam’s efficacy against β-lactamase enzymes.
Pharmacokinetic and Pharmacodynamic Considerations
CNS Penetration of Antibiotics
| Antibiotic | CSF Penetration (Inflamed Meninges) | Notes |
|---|---|---|
| Cefepime | ~10%–20% | Time-dependent, needs frequent dosing |
| Meropenem | ~20%–40% | High CNS activity |
| Colistin (IV) | <5% | Intraventricular preferred |
| Ceftazidime | ~20%–30% | Effective in combination |
| Amikacin (IV) | Poor | Use intrathecally |
| Fosfomycin | Variable | Synergy enhancer, esp. with cephalosporins |
Clinical Evidence Supporting Synergistic Combinations
- In vitro synergy testing (e.g., checkerboard assays, time-kill curves) demonstrates that meropenem and colistin exhibit >90% synergy against MDR P. aeruginosa CNS isolates.
- Case series involving intraventricular colistin plus ceftazidime have reported up to 80% microbiological clearance in patients with ventriculitis.
- Amikacin intrathecal administration, when paired with systemic β-lactams, reduces bacterial load in CSF by more than 3-log CFU/mL in experimental models.
Role of Intraventricular and Intrathecal Therapy
Because many agents do not reach effective CSF concentrations, direct CNS administration is often necessary:
- Indications:
- Multidrug-resistant strains
- Poor systemic drug penetration
- Persistent infection despite IV therapy
- Agents used:
- Colistin: 10 mg daily intraventricular
- Amikacin: 10–30 mg daily intrathecal
- Tobramycin or gentamicin: weight-based intraventricular dosing
- Monitoring:
- Serial CSF cultures
- Clinical improvement (neurological status)
- Renal and neurologic toxicity (neurotoxicity risk with colistin)
Surgical and Supportive Measures
- Device removal/replacement: Necessary in EVD or shunt-associated infections
- CSF drainage and lavage: Assists in reducing bacterial load
- ICP monitoring and management: Elevated intracranial pressure is a common complication
Duration of Therapy and Follow-Up
- Minimum of 14–21 days of treatment recommended, depending on:
- Organism susceptibility
- Clinical response
- CSF sterilization timing
- Therapy should continue for at least 10–14 days beyond the first negative CSF culture.
- Follow-up includes:
- Repeat lumbar punctures to assess sterilization
- Monitoring for relapse or treatment-associated toxicity
- Long-term neurological evaluation
Emerging Therapies and Future Directions
Cefiderocol in CNS Infections
- A novel siderophore cephalosporin active against XDR P. aeruginosa.
- Limited data on CSF penetration but promising in salvage therapy.
Bacteriophage Therapy
- Engineered phages targeting Pseudomonas biofilms show efficacy in preclinical CNS models.
- May be combined with traditional antibiotics in refractory meningitis.
Personalized Synergy Testing
- Rapid diagnostics (e.g., qPCR, resistance gene profiling) and customized synergy panels allow tailored therapy based on isolate characteristics.
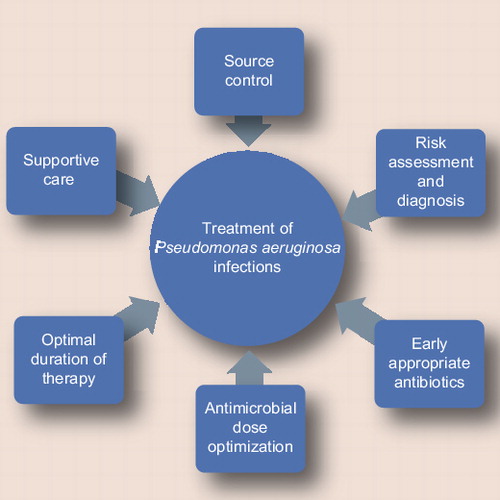
Strategic Combination Therapy for Effective Meningitis Management
Treatment of Pseudomonas aeruginosa meningitis requires more than empirical antibiotics; it necessitates a synergy-driven, targeted approach that accounts for CNS drug penetration, resistance mechanisms, and patient-specific factors. By leveraging effective combination regimens such as meropenem with colistin, ceftazidime with aminoglycosides, and novel agents like cefiderocol, we can significantly improve outcomes in this high-stakes clinical scenario. Early device removal, intrathecal administration when necessary, and rigorous follow-up remain essential pillars of successful intervention.

