Enterococcal endocarditis represents a formidable clinical challenge, particularly in patients with underlying valvular disease or indwelling medical devices. Enterococcus faecalis, the predominant species, accounts for nearly 10% of all infective endocarditis cases. These infections are difficult to treat due to the organism’s intrinsic resistance to many antibiotics and its ability to form biofilms on cardiac valves.
Preventing enterococcal endocarditis requires precise prophylactic strategies, especially in high-risk individuals undergoing procedures that predispose them to bacteremia. Synergistic antibiotic therapy offers a critical means of enhancing antimicrobial efficacy and overcoming the organism’s natural tolerance to monotherapy.
Pathophysiology of Enterococcal Infections and Endocarditis Risk
Enterococcus faecalis and Enterococcus faecium are part of the normal gastrointestinal flora but can become opportunistic pathogens when mucosal barriers are disrupted. Invasive procedures such as gastrointestinal surgeries, urological interventions, or dental manipulations can lead to transient bacteremia, seeding damaged endothelium or prosthetic cardiac material.
Key factors contributing to endocarditis include:
- Adherence to fibrin-platelet thrombi
- Biofilm formation on cardiac valves or prostheses
- Subacute presentation delaying diagnosis
- Resistance to host immune clearance
Because of the organism’s tolerance to cell wall-active agents like ampicillin or vancomycin alone, synergistic combinations are often essential for bactericidal action, particularly in prophylactic contexts.
Antibiotic Synergy in Enterococcal Prophylaxis: Mechanistic Insights
The hallmark of synergistic therapy against enterococci lies in combining a cell wall-active agent (such as a β-lactam) with an aminoglycoside. This exploits the enhanced uptake of the aminoglycoside due to the disruption of cell wall integrity, resulting in more effective intracellular action.
Key Mechanisms of Synergy:
- Cell wall inhibitors (ampicillin, vancomycin) open peptidoglycan pathways.
- Aminoglycosides (gentamicin, streptomycin) inhibit ribosomal protein synthesis after facilitated entry.
- Time-dependent killing by β-lactams complements the concentration-dependent bactericidal effect of aminoglycosides.
This dual-action not only ensures bactericidal activity but also reduces the risk of persistent bacteremia and vegetation formation in early phases.
Standard Synergistic Antibiotic Regimens for Prophylaxis
Ampicillin Plus Gentamicin
Ampicillin targets the cell wall, while gentamicin, once inside, disrupts bacterial protein synthesis.
- Recommended for high-risk cardiac patients undergoing procedures involving GI or GU tracts.
- Dosage: Ampicillin 2g IV plus gentamicin 1.5 mg/kg IV, ideally administered 30 minutes before procedure.
Vancomycin Plus Gentamicin
Used for patients allergic to β-lactams or infected with high-level β-lactam-resistant strains.
- Limitations: Increased nephrotoxicity; requires renal function monitoring.
- Avoid in patients with high-level aminoglycoside resistance.
Ceftriaxone Plus Ampicillin
For strains susceptible to ampicillin but in patients with aminoglycoside toxicity risks.
- Mechanism: Dual β-lactam synergy enhances PBP binding and cell wall inhibition.
- Efficacy: Demonstrated bactericidal activity without aminoglycoside-associated risks.
Prophylactic Indications: Identifying High-Risk Patients
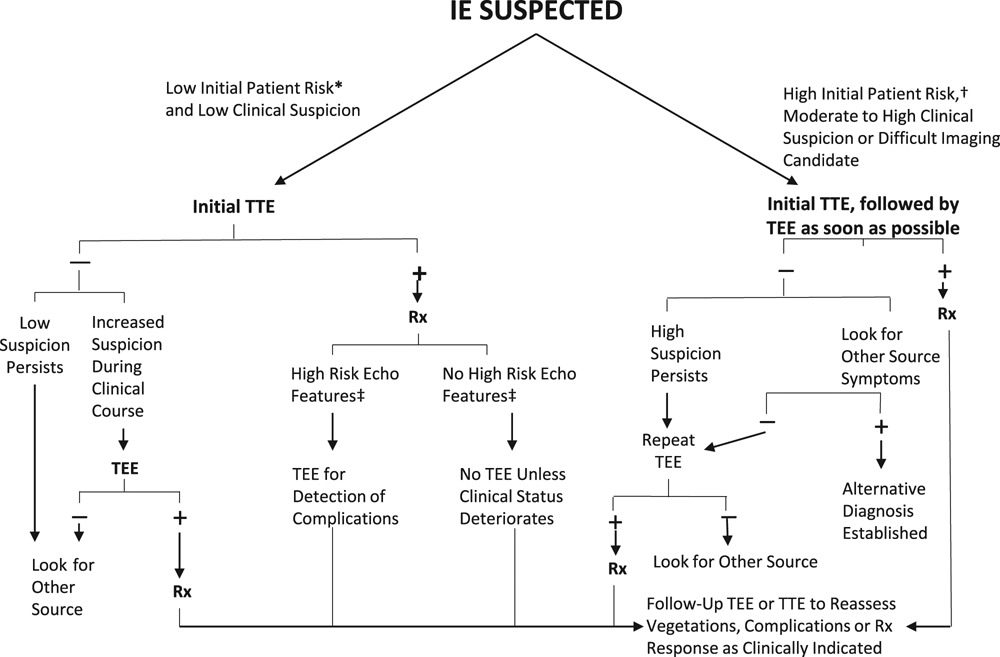
According to the American Heart Association (AHA) guidelines, prophylactic antibiotics are indicated for a limited subset of patients undergoing invasive procedures:
Cardiac Conditions That Require Prophylaxis:
- Prosthetic heart valves or prosthetic material used for valve repair
- Previous history of infective endocarditis
- Certain congenital heart diseases (CHD)
- Cardiac transplant recipients with valvulopathy
Procedures at Risk for Bacteremia:
- Dental procedures involving gingival tissue or perforation of oral mucosa
- Invasive respiratory or GI procedures in high-risk individuals
- Genitourinary manipulation in the presence of active infection
Emerging Challenges: Resistance and High-Level Aminoglycoside Resistance (HLAR)
One of the most pressing concerns in enterococcal prophylaxis is the emergence of HLAR, which nullifies the synergy between aminoglycosides and cell wall agents.
Mechanisms of HLAR:
- Acquisition of modifying enzymes (e.g., AAC(6′)-APH(2”))
- Mutations in 30S ribosomal subunit
- Reduced aminoglycoside uptake despite cell wall compromise
Alternative Approaches:
- Linezolid or Daptomycin: Though not standard for prophylaxis, these are critical for treatment in HLAR infections.
- High-dose dual β-lactam therapy: Effective alternative when aminoglycosides are contraindicated.
Role of Biofilm and Endothelial Adhesion in Prevention Failure
Biofilm formation significantly contributes to antibiotic tolerance and failure of prophylaxis. Enterococci express aggregation substance and adhesins that facilitate colonization and biofilm production on damaged endocardium.
Preventive strategies must focus on:
- Early eradication of bacteremia
- Inhibition of adhesion via anti-virulence agents (future scope)
- Targeted pre-operative antibiotic selection based on colonization profiles
Clinical Evidence Supporting Synergistic Prophylaxis
Several studies highlight the value of synergistic combinations in both prophylaxis and early treatment:
- Mohamed et al. (2022): Demonstrated reduced procedural bacteremia with ampicillin + gentamicin versus monotherapy.
- EUCAST breakpoints and in vitro time-kill assays: Consistently show ≥2-log CFU reduction when synergy is employed.
- Retrospective cardiac surgery reviews: Lower incidence of postoperative enterococcal endocarditis in patients who received synergistic regimens preoperatively.
Recommendations for Clinical Practice
- Evaluate individual risk profiles before deciding on prophylactic regimens.
- Perform susceptibility testing for enterococcal colonization when feasible.
- Use cell wall-active + aminoglycoside combinations for high-risk cases unless HLAR is detected.
- Consider β-lactam dual therapy as a safer alternative in elderly or renally impaired patients.
- Monitor renal function and serum levels when aminoglycosides are employed.
Optimizing Synergy to Prevent Enterococcal Endocarditis
Preventing enterococcal endocarditis in high-risk patients necessitates a proactive, evidence-based approach centered on synergistic antibiotic prophylaxis. Ampicillin-gentamicin remains the gold standard, but alternative strategies must be tailored in the context of resistance, allergy, and patient comorbidities. Integrating these regimens into preoperative protocols and adhering to current guideline-based recommendations are essential for minimizing the burden of this challenging infection.