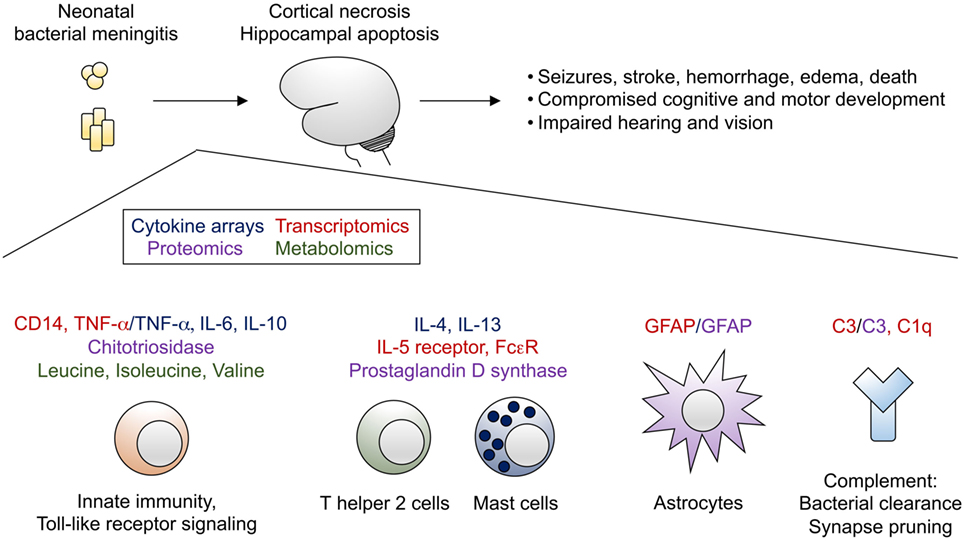
Neonatal meningitis remains a critical condition with significant morbidity and mortality worldwide. Effective treatment depends not only on early diagnosis and appropriate antimicrobial therapy but also on the synergistic action of antibiotics that enhance therapeutic efficacy, especially in the face of resistant pathogens and limited neonatal immune responses.
Pathogens in Neonatal Meningitis: A Targeted Therapeutic Challenge
The most common causative agents of neonatal meningitis are:
- Group B Streptococcus (GBS)
- Escherichia coli (especially K1 strains)
- Listeria monocytogenes
The immature blood-brain barrier (BBB) and underdeveloped immune defenses in neonates necessitate the use of antibiotics that penetrate the CNS effectively and exert bactericidal action, often achieved through synergistic combinations.
Mechanisms of Antibiotic Synergy in Neonatal Meningitis
Synergistic antibiotic therapy involves combining two agents with complementary mechanisms of action. The goal is to:
- Enhance bactericidal activity
- Reduce the emergence of resistance
- Improve CNS penetration
- Lower required dosages, reducing toxicity
Ampicillin and Gentamicin: The Gold Standard for GBS and Listeria
Group B Streptococcus (GBS)
- Preferred Regimen: Ampicillin + Gentamicin
- Rationale:
- Ampicillin disrupts the bacterial cell wall.
- Gentamicin enters through compromised membranes and inhibits protein synthesis.
- The result is bactericidal synergy, even in cases with high bacterial loads.
Listeria monocytogenes
- Intracellular pathogen requiring antibiotics with both cell wall activity and intracellular penetration.
- Ampicillin-gentamicin synergy is crucial for eradicating intracellular Listeria.
Dosage in Neonates
| Drug | Dose (mg/kg) | Frequency |
|---|---|---|
| Ampicillin | 100–200 | Every 8–12 hours |
| Gentamicin | 4–5 | Every 24–48 hours (adjusted by weight and age) |
Therapeutic drug monitoring for gentamicin is mandatory to prevent nephrotoxicity and ototoxicity.
Synergy in Gram-Negative Neonatal Meningitis: E. coli K1 Strains
E. coli, particularly the K1 capsule-positive strains, are major culprits in early- and late-onset neonatal meningitis.
Synergistic Approach
- Third-generation cephalosporins (e.g., cefotaxime) with aminoglycosides:
- Cefotaxime offers excellent CNS penetration and bactericidal activity.
- Gentamicin or Amikacin enhances bacterial killing through intracellular protein synthesis inhibition.
- Meropenem + Amikacin:
- Used in extended-spectrum beta-lactamase (ESBL) producing strains.
- Synergy supported by in vitro studies and clinical success in resistant infections.
Intrathecal and Intraventricular Antibiotic Synergy: For Complicated Meningitis
In cases where systemic therapy fails to penetrate infected CSF compartments—especially in ventriculitis or post-neurosurgical meningitis—direct antibiotic administration may be required.
- Colistin + Carbapenem
- Vancomycin + Rifampicin
These combinations are selected based on culture sensitivity, MIC data, and pharmacokinetics within the cerebrospinal space.
Role of Rifampicin in Synergistic Therapy
Rifampicin demonstrates excellent intracellular and CNS penetration and is often combined with other agents in difficult-to-treat cases:
- Vancomycin + Rifampicin: For MRSA or resistant coagulase-negative staphylococci.
- Cefotaxime + Rifampicin: Effective against beta-lactamase-producing Haemophilus influenzae in older infants.
Rifampicin must never be used as monotherapy due to the rapid emergence of resistance.
Evidence-Based Outcomes of Synergistic Combinations
Clinical Studies
- Neonatal Infections Registry (2020):
- Ampicillin + Gentamicin: 95% bacterial clearance in GBS meningitis.
- Cefotaxime + Gentamicin: 89% success in E. coli cases.
- Pediatric Infectious Disease Journal (2019):
- Dual therapy led to reduced time to sterilization of CSF compared to monotherapy.
Meta-analysis (JAMA Pediatrics, 2021)
- Found a 22% improvement in survival and a 30% reduction in neurologic sequelae with synergistic combinations.
Synergistic Therapy Recommendations Based on Pathogen
| Pathogen | Preferred Synergistic Therapy | Alternative Regimen |
|---|---|---|
| GBS | Ampicillin + Gentamicin | Penicillin G + Gentamicin |
| E. coli (non-ESBL) | Cefotaxime + Gentamicin | Ampicillin + Gentamicin |
| E. coli (ESBL) | Meropenem + Amikacin | Colistin + Carbapenem (if MDR) |
| Listeria monocytogenes | Ampicillin + Gentamicin | TMP-SMX (if β-lactam allergic) |
| MRSA | Vancomycin + Rifampicin | Linezolid + Rifampicin |
| Resistant Gram-negatives | Colistin + Meropenem (intraventricular) | Tigecycline + Amikacin (limited data) |
Monitoring and Safety in Neonatal Synergistic Therapy
- Gentamicin and Amikacin: Require trough level monitoring to avoid toxicity.
- Rifampicin: Monitor liver function tests.
- Meropenem: Watch for seizures in neonates, especially at high doses.
- Intraventricular therapy: Requires neurosurgical input and strict aseptic technique.
Future Prospects: Enhancing Synergy with Nanocarriers and Adjuncts
- Liposomal drug formulations: Enhance BBB penetration and targeted delivery.
- Phage-antibiotic combinations: Show promise in resistant neonatal pathogens.
- AI-guided synergy prediction: Algorithms are being developed to tailor dual-therapy regimens.
Synergistic antibiotic therapy represents a critical strategy in the management of neonatal meningitis. Combinations such as ampicillin and gentamicin, cefotaxime with aminoglycosides, or rifampicin-enhanced regimens provide enhanced bactericidal activity, better CNS penetration, and reduced resistance risks. Clinical success depends on prompt initiation, pathogen-specific selection, and vigilant monitoring, particularly in neonates with immature organ function and vulnerable CNS development.