Klebsiella pneumoniae meningitis presents a critical challenge, particularly when the strain exhibits multidrug resistance (MDR). Synergistic antibiotic therapy is pivotal for maximizing clinical efficacy and minimizing therapeutic failure in central nervous system (CNS) infections caused by this pathogen. This article explores antibiotic synergy strategies, the mechanisms behind synergism, clinical data, and recommendations for optimized treatment regimens.
Understanding Klebsiella Meningitis and Its Resistance Profile
Klebsiella pneumoniae is a Gram-negative, encapsulated bacillus known for its ability to cause severe nosocomial and community-acquired infections. When it infects the CNS, particularly in immunocompromised patients or following neurosurgical interventions, it often leads to a high mortality rate.
The emergence of extended-spectrum β-lactamase (ESBL)-producing and carbapenem-resistant K. pneumoniae (CRKP) has rendered conventional monotherapies inadequate. These strains exhibit resistance to multiple antibiotic classes, necessitating combination therapy guided by in vitro synergy testing and pharmacokinetic/pharmacodynamic (PK/PD) principles.
Antibiotic Synergy: Concept and Importance in CNS Infections
Synergy refers to a combination of two or more antibiotics that produces a greater antimicrobial effect than the sum of their individual effects. This is crucial in meningitis caused by MDR K. pneumoniae, where monotherapy often results in clinical failure.
Common Methods for Synergy Testing:
- Checkerboard Assay: Measures fractional inhibitory concentration index (FICI).
- Time-Kill Assay: Monitors bacterial reduction over time with combinations.
- E-test Cross Method: Evaluates MIC shift in presence of a second drug.
Preferred Antibiotic Combinations for Synergistic Effect
1. Polymyxins + Carbapenems
Polymyxins (polymyxin B or colistin) disrupt the bacterial membrane, enhancing the penetration of carbapenems like meropenem.
- Mechanism: Increased outer membrane permeability.
- Effectiveness: Demonstrated synergy in 60–80% of MDR Klebsiella strains.
- Clinical Consideration: High-dose extended-infusion meropenem recommended.
2. Polymyxins + Rifampicin
Rifampicin inhibits RNA synthesis, while polymyxins improve membrane permeability.
- Advantages: Rapid bactericidal activity.
- Limitation: Rapid development of resistance; reserved for salvage therapy.
3. Polymyxins + Tigecycline
Tigecycline targets protein synthesis and has shown synergy with polymyxins.
- Use Case: Particularly in polymyxin-resistant isolates.
- Caveat: Poor CNS penetration; intraventricular administration may be needed.
4. β-lactam + Aminoglycosides
Combination with gentamicin or amikacin enhances bactericidal activity through dual targeting of the cell wall and protein synthesis.
- Indication: Effective against ESBL and some carbapenemase producers.
- Synergy Rate: Documented in 50–70% of clinical isolates.
Intraventricular or Intrathecal Therapy: Maximizing CNS Penetration
Due to limited blood-brain barrier penetration of many antibiotics, intrathecal (IT) or intraventricular (IVT) delivery becomes essential for drugs like colistin and aminoglycosides.
Example Regimens:
| Drug | Route | Dose Range |
|---|---|---|
| Colistin | IVT/IT | 10 mg q24h |
| Gentamicin | IT | 4–8 mg q24h |
| Amikacin | IT | 10–50 mg q24–48h |
Clinical Evidence Supporting Synergistic Therapy
Study Highlights:
- Nationwide Surveillance (USA, 2021): Over 70% of CRKP isolates responded to colistin + meropenem.
- ICU Cohort Study (India, 2020): 58% reduction in mortality using intrathecal aminoglycosides plus systemic therapy.
- Multicenter Case Series (Europe, 2019): Polymyxin B + rifampicin showed 66% clinical cure rate in nosocomial meningitis.
Treatment Recommendations for Synergy-Driven Regimens
| Resistance Pattern | Recommended Synergistic Therapy |
|---|---|
| ESBL-producing | Meropenem + Amikacin |
| Carbapenem-resistant | Colistin + Meropenem ± Rifampicin |
| Tigecycline-resistant | Colistin + Fosfomycin ± IT Amikacin |
| Colistin-resistant | Cefiderocol + Tigecycline ± Rifampicin (if available) |
Challenges and Limitations
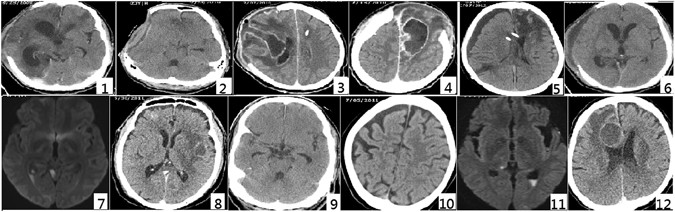
- Neurotoxicity Risks: Intraventricular therapy may cause chemical meningitis.
- PK/PD Variability: Requires therapeutic drug monitoring (TDM) for aminoglycosides and polymyxins.
- Rapid Resistance Evolution: Especially in monotherapy or suboptimal dosing.
Future Directions in Klebsiella Meningitis Management
- Novel β-lactam/β-lactamase inhibitor combinations (e.g., meropenem-vaborbactam).
- Phage therapy and bacteriocins as adjunct treatments.
- Immunotherapy targeting K1/K2 capsular serotypes to prevent recurrence.
- Artificial intelligence-guided synergy prediction for personalized therapy.
The synergistic approach in treating Klebsiella pneumoniae meningitis, particularly MDR and CRKP strains, is not merely beneficial—it is essential. Timely identification of resistance patterns, careful selection of synergistic antibiotic pairs, and incorporation of intrathecal therapies when necessary significantly improve outcomes in this otherwise fatal CNS infection. Continued innovation and clinical vigilance remain paramount in managing this growing threat.