Citrobacter species, particularly Citrobacter freundii, are opportunistic pathogens that can cause meningitis in both immunocompromised individuals and those with other predisposing conditions such as trauma, neurosurgery, or underlying chronic diseases. Although less common than other causative agents of bacterial meningitis, Citrobacter meningitis presents a significant clinical challenge due to its potential for antibiotic resistance and the complex management it necessitates.
In this article, we explore the critical aspects of synergy in the treatment of Citrobacter meningitis, focusing on antibiotic combinations, adjunctive therapies, and management strategies to improve patient outcomes and reduce the risk of complications.
The Pathogenesis of Citrobacter Meningitis
Citrobacter meningitis typically occurs when Citrobacter species invade the central nervous system (CNS), often as a consequence of hematogenous spread or direct contamination through surgical procedures. The ability of Citrobacter species to produce beta-lactamase and their inherent resistance to certain antibiotics complicate treatment regimens. The most common strains associated with meningitis include Citrobacter freundii, which can be resistant to a broad range of antibiotics, necessitating the use of combination therapy.
Risk Factors for Citrobacter Meningitis
Key risk factors for developing Citrobacter meningitis include:
- Premature infants and neonates, who are more susceptible to CNS infections due to underdeveloped immune systems.
- Neurological surgeries or head trauma, which can facilitate bacterial entry into the CNS.
- Immunocompromised states, such as those resulting from HIV/AIDS, chemotherapy, or organ transplants.
- Underlying comorbidities, including diabetes and chronic kidney disease, which may predispose individuals to infections.
Antibiotic Therapy for Citrobacter Meningitis
Effective treatment of Citrobacter meningitis often involves the use of multiple antibiotics in synergy to overcome bacterial resistance mechanisms. Citrobacter species can exhibit resistance to several classes of antibiotics, including penicillins, cephalosporins, and fluoroquinolones. Therefore, antibiotic synergy plays a critical role in enhancing the bactericidal effect and ensuring comprehensive coverage against the pathogen.
Common Antibiotics for Citrobacter Meningitis
Several antibiotics have shown efficacy in the treatment of Citrobacter meningitis, often in combination:
- Ceftriaxone or Cefotaxime: Third-generation cephalosporins are typically the first-line treatment, effective against many Gram-negative organisms, including Citrobacter.
- Meropenem: A carbapenem antibiotic that is particularly effective against extended-spectrum beta-lactamase (ESBL)-producing strains of Citrobacter.
- Vancomycin: Although primarily used for Gram-positive infections, vancomycin may be used in combination to provide broader spectrum coverage in cases of suspected co-infections.
- Gentamicin: This aminoglycoside can be added to augment the effects of beta-lactams, particularly in treating serious infections like meningitis.
Synergistic Antibiotic Combinations
Antibiotic synergy occurs when two or more drugs work together to provide a greater bactericidal effect than would be expected from their individual actions. In the context of Citrobacter meningitis, the following synergistic combinations are commonly employed:
- Ceftriaxone + Gentamicin: This combination leverages ceftriaxone‘s ability to inhibit bacterial cell wall synthesis and gentamicin‘s mechanism of inhibiting protein synthesis. Together, they provide broad-spectrum coverage, targeting both the cell wall and the protein synthesis processes within the bacteria.
- Meropenem + Vancomycin: Meropenem, a broad-spectrum carbapenem, targets Citrobacter’s cell wall synthesis, while vancomycin can inhibit Gram-positive organisms, including any possible Staphylococcus aureus co-infections, providing comprehensive coverage for resistant strains.
- Cefotaxime + Trimethoprim-Sulfamethoxazole: This combination has proven effective in treating complicated Citrobacter infections, particularly in neonates and immunocompromised patients. The synergy between cefotaxime and trimethoprim-sulfamethoxazole helps overcome resistance and ensures effective treatment for this pathogen.
Adjunctive Therapies for Citrobacter Meningitis
In addition to antibiotic therapy, adjunctive treatments are often employed to address inflammation, support the immune system, and mitigate complications associated with meningitis.
Corticosteroids: A Role in Inflammation Control
Corticosteroids, such as dexamethasone, are often used in bacterial meningitis to reduce inflammation within the brain and spinal cord. This adjunctive therapy is particularly beneficial in preventing long-term neurological sequelae, such as hearing loss and cognitive impairment, commonly associated with meningococcal and pneumococcal meningitis. However, their role in Citrobacter meningitis remains debated, with current evidence suggesting that they may not have the same level of benefit as with other bacterial pathogens.
Hypertonic Saline and Mannitol for Increased Intracranial Pressure (ICP)
For patients experiencing elevated intracranial pressure (ICP), the use of hypertonic saline or mannitol may be employed to reduce cerebral edema. This is crucial for preventing further neurological damage, particularly in severe cases of bacterial meningitis. The use of these agents can be combined with antibiotic treatment to provide comprehensive care.
Supportive Care: Fluid and Electrolyte Balance
Fluid management is essential to prevent dehydration and maintain electrolyte balance during treatment. Proper hydration helps ensure adequate blood flow to vital organs, including the brain, and supports the body’s immune system. Careful monitoring of renal function is also important, as some antibiotics, such as gentamicin, can be nephrotoxic.
Diagnosis of Citrobacter Meningitis
The timely and accurate diagnosis of Citrobacter meningitis is essential for guiding treatment decisions and improving patient outcomes. The diagnostic process typically involves a combination of clinical evaluation, laboratory testing, and imaging studies.
Clinical Presentation of Citrobacter Meningitis
Patients with Citrobacter meningitis usually present with classic symptoms of bacterial meningitis, including:
- Fever
- Severe headache
- Nausea and vomiting
- Stiff neck
- Photophobia
- Altered mental status (e.g., confusion, drowsiness)
Lumbar Puncture (LP) and Cerebrospinal Fluid (CSF) Analysis
The lumbar puncture is the primary diagnostic tool for confirming bacterial meningitis. CSF analysis typically reveals:
- Elevated white blood cell count (pleocytosis)
- Low glucose levels (due to bacterial consumption of glucose)
- High protein levels (reflecting inflammation)
- Positive culture or PCR results for Citrobacter species
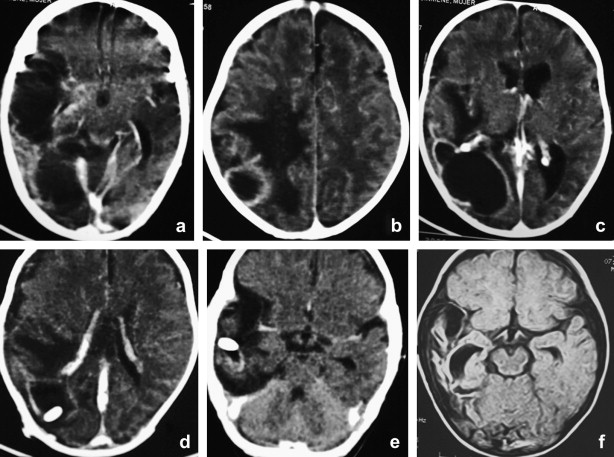
Blood cultures and imaging studies such as CT or MRI scans may also be performed to assess complications or identify sources of infection.
Prognosis and Long-Term Management
The prognosis for Citrobacter meningitis depends on several factors, including the timing of diagnosis, the effectiveness of treatment, and the presence of underlying health conditions. Early diagnosis and appropriate antibiotic therapy significantly improve patient outcomes.
Neurological Sequelae
Despite aggressive treatment, some patients may experience long-term complications, such as:
- Cognitive impairments
- Hearing loss
- Seizures
- Motor dysfunction
The use of corticosteroids and other supportive therapies has been shown to help mitigate some of these long-term effects.
Effective management of Citrobacter meningitis requires a comprehensive approach that combines synergistic antibiotic therapy, adjunctive treatments, and supportive care. The synergy between different classes of antibiotics enhances the therapeutic effect, overcoming resistance and improving clinical outcomes. As antibiotic resistance continues to challenge treatment options, ongoing research into new therapeutic combinations and adjunctive therapies remains essential for improving the prognosis of patients with Citrobacter meningitis.
By understanding the complexities of Citrobacter meningitis and employing a synergistic treatment strategy, healthcare professionals can provide better care for individuals affected by this potentially devastating infection.

