Bacterial meningitis is a severe and life-threatening infection of the membranes surrounding the brain and spinal cord. It can be caused by a variety of bacteria, including Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae. Left untreated, bacterial meningitis can lead to severe neurological damage, long-term disabilities, and even death. Therefore, early diagnosis and prompt, effective treatment are critical.
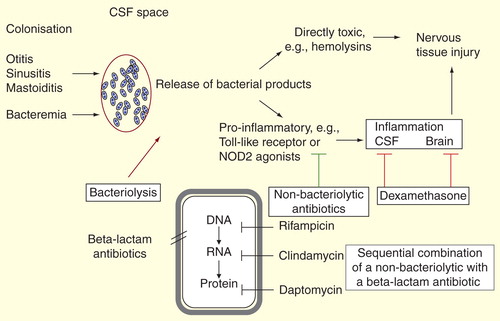
The concept of synergy in bacterial meningitis treatment revolves around the combined use of different therapeutic agents to enhance the overall effectiveness of therapy. This article explores the synergistic approaches that are integral to successfully managing bacterial meningitis, including antibiotic combinations, adjunctive therapies, and evolving treatment protocols.
The Role of Antibiotic Synergy in Bacterial Meningitis
Antibiotic therapy is the cornerstone of treatment for bacterial meningitis. However, the increasing prevalence of antibiotic resistance has led to the exploration of synergistic antibiotic combinations. Synergy occurs when two or more antibiotics work together to produce a greater effect than when used individually. In bacterial meningitis, this approach can help overcome bacterial resistance mechanisms, improve clinical outcomes, and reduce the risk of complications.
Common Antibiotics Used in Bacterial Meningitis
The choice of antibiotics depends on the causative organism, age of the patient, and local resistance patterns. Common antibiotics used include:
- Ceftriaxone or Cefotaxime: Broad-spectrum cephalosporins that target most pathogens causing meningitis.
- Vancomycin: Effective against resistant Streptococcus pneumoniae and Methicillin-resistant Staphylococcus aureus (MRSA).
- Ampicillin: Commonly used for Listeria monocytogenes, particularly in neonates and older adults.
- Penicillin G: Effective for Neisseria meningitidis and Streptococcus pneumoniae.
Synergistic Antibiotic Combinations
- Penicillin + Gentamicin: This combination is often used for Enterococcus infections. The synergy between penicillin, which targets the bacterial cell wall, and gentamicin, which inhibits protein synthesis, enhances the bactericidal effect.
- Ceftriaxone + Vancomycin: In cases of suspected methicillin-resistant Staphylococcus aureus (MRSA) meningitis, this combination provides broad coverage against resistant strains while targeting the cell wall synthesis and disrupting bacterial protein production.
- Meropenem + Linezolid: In cases of multi-drug resistant (MDR) pathogens, a combination of meropenem, a broad-spectrum carbapenem, and linezolid, an oxazolidinone antibiotic, can help combat resistant Gram-negative and Gram-positive bacteria.
These combinations aim to attack different bacterial targets, ensuring faster bacterial eradication, reducing the risk of treatment failure, and improving patient outcomes.
Adjunctive Therapies in Meningitis Treatment
While antibiotics form the primary line of defense, adjunctive therapies can significantly improve patient outcomes. These treatments, when used synergistically with antibiotics, help reduce inflammation, mitigate the effects of bacterial toxins, and support the body’s immune response.
Corticosteroids in Meningitis
The use of corticosteroids, particularly dexamethasone, has become standard practice in the treatment of bacterial meningitis, especially for Streptococcus pneumoniae meningitis. Dexamethasone works by reducing inflammation and preventing neurological damage caused by the host’s immune response to the infection. It also has the potential to improve long-term outcomes by reducing the risk of hearing loss and other neurological sequelae.
Hypertonic Saline for Elevated Intracranial Pressure
For patients with increased intracranial pressure (ICP), the administration of hypertonic saline can help reduce brain swelling. This therapy works synergistically with antibiotics and corticosteroids, promoting better intracranial pressure management and improving blood flow to the brain.
Supportive Care: Fluids and Electrolytes
Effective fluid management is essential for maintaining hemodynamic stability during treatment. IV fluids are administered to maintain hydration, correct electrolyte imbalances, and support renal function. Careful monitoring is required to avoid fluid overload, which can worsen cerebral edema and increase ICP.
Diagnosis of Bacterial Meningitis
The diagnosis of bacterial meningitis involves a combination of clinical assessment, laboratory testing, and imaging studies. Prompt diagnosis is crucial for initiating early treatment and preventing serious complications.
Clinical Presentation
Patients with bacterial meningitis often present with a sudden onset of symptoms, including:
- Fever
- Headache
- Neck stiffness
- Altered mental status (confusion, lethargy, or agitation)
Lumbar Puncture (LP)
Lumbar puncture is the gold standard for diagnosing meningitis. The cerebrospinal fluid (CSF) obtained during an LP is analyzed for signs of infection, including:
- Elevated white blood cell count (pleocytosis)
- Low glucose levels
- High protein levels
- Positive culture or PCR results for the causative bacteria
Blood Cultures and Imaging
Blood cultures are essential for identifying the causative organism and determining antibiotic sensitivity. CT or MRI scans may be used in cases of suspected complications, such as brain abscesses or severe cerebral edema.
Prevention and Vaccination
Preventing bacterial meningitis through vaccination is the most effective strategy to reduce the incidence of this life-threatening infection. Several vaccines are available to protect against common causes of bacterial meningitis, including:
- Meningococcal vaccines: Protect against Neisseria meningitidis strains A, C, W, and Y.
- Pneumococcal vaccines: Protect against Streptococcus pneumoniae, a leading cause of bacterial meningitis in both children and adults.
- Haemophilus influenzae type b (Hib) vaccine: Protects against Haemophilus influenzae, a common pathogen in young children.
In addition to vaccination, the use of prophylactic antibiotics in close contacts of individuals with bacterial meningitis can help prevent further spread of the infection.
Prognosis and Long-Term Management
The prognosis for bacterial meningitis has improved significantly with advances in early diagnosis and treatment. However, the disease remains a serious condition, with mortality rates ranging from 10-20%, depending on the causative organism and promptness of treatment.
Neurological Sequelae
Despite successful treatment, some patients may experience long-term neurological sequelae, including:
- Hearing loss
- Cognitive impairment
- Seizures
- Motor deficits
Early initiation of corticosteroids and appropriate antibiotic therapy reduces the likelihood of long-term complications.
Synergy in the treatment of bacterial meningitis is essential to improving patient outcomes and reducing the risk of complications. By combining antibiotics, adjunctive therapies, and supportive care, healthcare providers can offer a comprehensive approach to managing this life-threatening infection. Ongoing advancements in treatment protocols, the development of new therapeutic agents, and early vaccination efforts are pivotal in reducing the global burden of bacterial meningitis.
Maintaining high vigilance for antibiotic resistance and adapting treatment regimens to suit individual patient needs will continue to be key factors in achieving optimal results in bacterial meningitis management.