Syncope due to heart block refers to fainting episodes or loss of consciousness that occur when the heart’s electrical conduction system is impaired. Heart block, or atrioventricular (AV) block, disrupts the normal electrical impulses between the atria and ventricles, causing a delay or complete blockage in the transmission of signals that control the heartbeat. This dysfunction leads to bradycardia (slow heart rate), which in turn can cause inadequate blood flow to the brain, resulting in syncope.
Types of Heart Block
- First-degree AV block: Prolonged conduction time but no complete block.
- Second-degree AV block: Some electrical signals are blocked, leading to intermittent skipped heartbeats.
- Third-degree AV block (complete block): No electrical impulses pass from the atria to the ventricles, causing the ventricles to contract at an independent rate.
Causes of Heart Block
Structural Heart Disease
Heart block often results from structural changes in the heart that impair the normal function of the AV node or bundle of His. These include:
- Coronary artery disease (leading to myocardial infarction)
- Valvular heart disease (e.g., mitral valve disease)
- Cardiomyopathies (e.g., dilated or hypertrophic cardiomyopathy)
- Endocarditis or other infections affecting the conduction system
Age-Related Degeneration
With aging, there is a natural degeneration of the heart’s conduction tissue, increasing the risk of heart block, especially in those over 60 years old.
Medications and Drugs
Certain medications can interfere with heart conduction, including:
- Beta-blockers and calcium channel blockers
- Digoxin, a medication for heart failure
- Antiarrhythmic drugs like amiodarone
- Tricyclic antidepressants and opioids (in overdose)
Electrolyte Imbalances
Imbalances in potassium, calcium, or magnesium can disrupt the electrical conduction system, leading to heart block.
Autonomic Nervous System Dysfunction
Conditions like sleep apnea, vasovagal syncope, or autonomic neuropathy may lead to heart block due to autonomic tone fluctuations.
Symptoms of Syncope Due to Heart Block
The hallmark symptom of syncope due to heart block is sudden fainting or near-fainting episodes. However, individuals may also experience:
- Dizziness or lightheadedness before fainting
- Palpitations or a sensation of a slow or irregular heartbeat
- Fatigue or weakness following an episode
- Confusion after regaining consciousness
- Shortness of breath in more severe cases
The severity of these symptoms depends on the degree of heart block and the heart rate during the episode. A complete block can cause sudden and profound syncope, while a partial block may result in intermittent lightheadedness.
Diagnosing Heart Block-Related Syncope
The diagnosis of syncope due to heart block relies on a thorough clinical evaluation and electrocardiogram (ECG). Key diagnostic steps include:
1. Medical History and Symptom Assessment
A detailed patient history is essential to determine potential triggers or predisposing conditions. Symptoms such as the frequency, duration, and circumstances of fainting episodes can help guide the diagnosis.
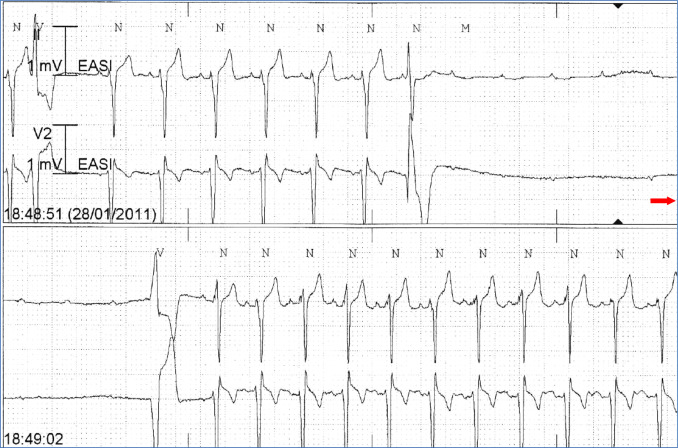
2. Electrocardiogram (ECG)
An ECG is the primary diagnostic tool used to evaluate heart rhythm and detect heart block. The findings may show prolonged PR intervals (in first-degree block), dropped QRS complexes (in second-degree block), or complete dissociation between atrial and ventricular activity (in third-degree block).
3. Holter Monitor
For intermittent symptoms, a 24-hour Holter monitor may be used to record the heart’s activity over time, helping detect episodes of heart block that do not appear during a standard ECG.
4. Electrophysiological Study (EPS)
In certain cases, an EPS can be performed to evaluate the electrical conduction system of the heart in detail. This procedure involves inserting electrodes into the heart to assess the conduction pathways and identify specific areas of dysfunction.
Treatment of Syncope Due to Heart Block
The management of syncope due to heart block is primarily focused on restoring normal electrical conduction and preventing recurrent fainting episodes. Treatment strategies depend on the type and severity of the heart block.
1. Pharmacologic Treatment
In mild cases of heart block, medications may be prescribed to regulate heart rate and improve conduction:
- Atropine: In cases of acute symptomatic bradycardia, atropine can be administered to increase the heart rate.
- Beta-agonists: These may be used to improve conduction in certain types of heart block.
2. Pacemaker Implantation
For second-degree or third-degree heart block, especially when symptomatic, the most effective treatment is the implantation of a permanent pacemaker. The pacemaker ensures that the heart rate is maintained by artificially stimulating the heart to beat at an appropriate rate. Pacemakers are particularly useful for preventing recurrent syncope and improving the quality of life.
3. Lifestyle Modifications
In addition to medical treatment, lifestyle changes such as avoiding triggers (e.g., dehydration, certain medications) can help manage symptoms and reduce the risk of syncope. Increasing fluid intake and avoiding standing for long periods can alleviate the symptoms.
4. Management of Underlying Conditions
In cases where heart block is secondary to conditions like myocardial infarction, valvular heart disease, or cardiomyopathy, treating the underlying cause may improve the symptoms of syncope. This could include surgical interventions, such as coronary artery bypass grafting (CABG) or valve replacement, as appropriate.
Prognosis and Long-Term Management
The long-term prognosis for individuals with syncope due to heart block varies depending on the underlying cause and severity of the block. Patients with complete heart block (third-degree) require ongoing management with a pacemaker to prevent life-threatening consequences, such as sudden cardiac arrest. Those with milder forms of heart block may lead normal lives with medication and lifestyle adjustments.
Regular follow-up visits are essential to monitor the function of the pacemaker and ensure there are no complications, such as infection or lead dislodgement.
Preventing Recurrence of Syncope
While pacemaker therapy provides a reliable solution for many, lifestyle modifications are crucial to prevent recurrent episodes of syncope. Measures include:
- Avoiding sudden postural changes (e.g., standing up too quickly)
- Limiting the intake of substances that exacerbate bradycardia, such as alcohol and certain medications
- Ensuring adequate hydration, particularly in warm environments
Syncope due to heart block is a significant medical condition that warrants timely diagnosis and treatment to prevent further complications. By recognizing the symptoms, understanding the underlying causes, and implementing effective management strategies, patients can effectively mitigate the risks associated with heart block and improve their quality of life.
For individuals with more severe forms of heart block, pacemaker implantation remains the gold standard for preventing syncope and ensuring long-term cardiac stability. Regular medical follow-up is essential to monitor heart health and prevent further episodes. With the appropriate care, patients can lead active and fulfilling lives.

