Symptomatic orthostatic hypotension (OH) is a clinically significant drop in blood pressure upon standing, accompanied by symptoms such as dizziness, lightheadedness, visual disturbances, fatigue, or even syncope. The condition is defined by a sustained reduction of at least 20 mmHg in systolic or 10 mmHg in diastolic pressure within three minutes of standing or head-up tilt. It reflects a failure in the autonomic nervous system to regulate vascular tone and heart rate appropriately.
Pathophysiology of Orthostatic Hypotension
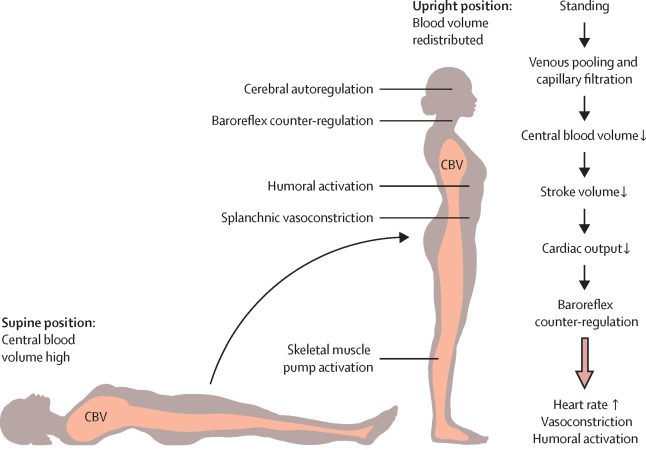
Orthostatic hypotension results from inadequate autonomic reflex responses to gravitational blood shifts. Upon standing, approximately 500 to 1000 mL of blood pools in the lower extremities, decreasing venous return to the heart and lowering cardiac output. In a healthy individual, baroreceptors trigger vasoconstriction and tachycardia to compensate. In OH, these reflexes fail.
Primary Mechanisms:
- Impaired baroreflex sensitivity
- Autonomic nervous system dysfunction
- Reduced intravascular volume
- Delayed vasoconstriction or neurogenic failure
Common Symptoms of Symptomatic Orthostatic Hypotension
Symptoms typically occur within minutes of standing and may vary in severity based on the underlying cause. They include:
- Lightheadedness or dizziness
- Blurred or tunnel vision
- Generalized weakness
- Fatigue after exertion
- Palpitations or chest discomfort
- Syncope (fainting), particularly in severe cases
These symptoms often worsen in the morning, after meals, with heat exposure, or following prolonged standing.
Etiological Classification of Orthostatic Hypotension
Neurogenic Causes
Often linked to autonomic nervous system failure, particularly in neurodegenerative diseases:
- Parkinson’s disease
- Multiple system atrophy
- Pure autonomic failure
- Diabetic autonomic neuropathy
- Amyloidosis
Non-Neurogenic Causes
Secondary to hypovolemia or medications:
- Dehydration
- Hemorrhage
- Adrenal insufficiency
- Diuretic or antihypertensive use
- Prolonged bed rest or deconditioning
Diagnostic Criteria and Evaluation
A detailed patient history and physical examination form the cornerstone of diagnosis.
Orthostatic Vital Signs
- Measure blood pressure and heart rate supine and after 1, 3, and 5 minutes of standing.
- A diagnostic drop ≥20 mmHg systolic or ≥10 mmHg diastolic confirms OH.
Additional Diagnostic Tests
- Tilt-table test: For patients with unclear symptoms or suspected autonomic dysfunction.
- 24-hour Holter monitor: To assess heart rate variability and exclude arrhythmias.
- Autonomic function testing: Valsalva maneuver, deep breathing tests.
- Blood and urine tests: To identify metabolic or volume-related abnormalities.
Management of Symptomatic Orthostatic Hypotension
Treatment focuses on underlying cause correction, symptom relief, and prevention of complications like falls or syncope.
Non-Pharmacologic Interventions
Volume Expansion and Lifestyle Measures:
- Increased fluid intake (2.5–3 liters/day)
- Salt supplementation (6–10 grams/day if not contraindicated)
- Compression garments: Abdominal binders or thigh-high stockings
- Elevating head of bed: Minimizes nocturnal diuresis and morning hypotension
- Frequent small meals: Prevent postprandial hypotension
Behavioral Adjustments:
- Rise slowly from sitting or lying down
- Avoid prolonged standing and overheating
- Perform counter-pressure maneuvers (e.g., leg crossing, squatting)
Pharmacologic Therapies
If lifestyle changes are insufficient, medications may be introduced:
| Drug | Mechanism | Typical Dosage |
|---|---|---|
| Fludrocortisone | Expands plasma volume | 0.1–0.3 mg/day |
| Midodrine | Alpha-1 agonist, vasoconstrictor | 2.5–10 mg 3x/day |
| Droxidopa | Norepinephrine precursor | 100–600 mg 3x/day |
| Pyridostigmine | Acetylcholinesterase inhibitor | 30–60 mg 1–3x/day |
Monitoring for supine hypertension is essential when initiating therapy.
Prognosis and Long-Term Monitoring
The prognosis depends on the underlying cause. Neurogenic forms often progress with the primary disease, while secondary causes may resolve with appropriate treatment. Regular monitoring of blood pressure, symptom severity, and fall risk is necessary.
Patients require tailored care plans incorporating:
- Multidisciplinary support (neurology, cardiology, geriatrics)
- Periodic reevaluation of medications
- Fall risk mitigation strategies
- Education on symptom recognition and emergency protocols
Differentiating Orthostatic Hypotension from Similar Conditions
| Condition | Key Difference |
|---|---|
| Vasovagal Syncope | Triggered by emotional distress or pain, with bradycardia |
| POTS (Postural Orthostatic Tachycardia Syndrome) | HR increase ≥30 bpm without BP drop |
| Carotid Sinus Hypersensitivity | Triggered by neck movement or pressure |
| Hypoglycemia | Often accompanied by diaphoresis, hunger, and neurologic signs |
Accurate differentiation is vital for effective management.
Public Health Relevance and Clinical Impact
With an aging global population and rising prevalence of neurodegenerative diseases, symptomatic orthostatic hypotension is increasingly common. Unrecognized or undertreated OH significantly impacts quality of life, increases fall risk, and contributes to morbidity.
Early detection, proactive management, and patient education are key to improving outcomes and reducing healthcare burden.
Symptomatic orthostatic hypotension is a multifaceted condition requiring a comprehensive approach. Recognizing its symptoms, understanding the underlying physiology, and implementing appropriate therapeutic strategies are essential to reduce complications and improve patient outcomes. Long-term management demands a multidisciplinary strategy rooted in patient-specific interventions and regular reassessment.

