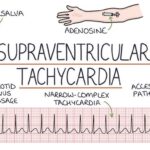
Supraventricular tachycardia (SVT) encompasses a group of arrhythmias characterized by an abnormally rapid heart rate originating above the ventricles. This condition can cause significant discomfort and functional impairment, particularly when episodes occur frequently or persist for extended periods. SVT is often paroxysmal, meaning it begins and ends abruptly.

Types of Supraventricular Tachycardia
SVT is a collective term for several specific arrhythmias, each with unique electrophysiological mechanisms:
1. Atrioventricular Nodal Reentrant Tachycardia (AVNRT)
- Most common SVT subtype.
- Caused by a reentrant circuit within or near the AV node.
- Typically presents in young adults.
2. Atrioventricular Reentrant Tachycardia (AVRT)
- Involves an accessory pathway outside the AV node.
- Classic example: Wolff-Parkinson-White (WPW) syndrome.
- Can result in dangerously high ventricular rates if associated with atrial fibrillation.
3. Atrial Tachycardia
- Arises from ectopic atrial foci independent of the sinus node.
- May be unifocal or multifocal.
- Often resistant to vagal maneuvers and medications.
4. Sinus Tachycardia and Inappropriate Sinus Tachycardia
- Originates from the sinus node.
- Inappropriate variant occurs without physiological stimuli, often in younger patients.
Pathophysiology: Reentry and Ectopic Focus Mechanisms
SVT arises due to one of the following:
- Reentry Circuits: Electrical impulses loop around abnormal conduction pathways, triggering rapid contractions.
- Automaticity: Spontaneous depolarization of ectopic pacemaker cells.
- Triggered Activity: Afterdepolarizations initiate premature beats, potentially leading to sustained arrhythmias.
Recognizing the Clinical Features of SVT
Common Symptoms:
- Palpitations (sudden onset and termination)
- Lightheadedness or dizziness
- Chest tightness or discomfort
- Dyspnea
- Syncope or near-syncope in severe cases
- Fatigue, especially post-episode
Symptom Duration:
- Seconds to hours; prolonged episodes may necessitate emergency care.
Risk Factors and Triggers
- Structural heart disease
- Congenital accessory pathways (e.g., WPW syndrome)
- Excessive caffeine, alcohol, or stimulant use
- Emotional stress or fatigue
- Hyperthyroidism
- Electrolyte imbalances (e.g., hypokalemia, hypomagnesemia)
- Post-surgical cardiac patients
Diagnostic Approach to Supraventricular Tachycardia
1. Electrocardiogram (ECG)
- Narrow QRS complexes (<120 ms)
- Heart rate typically between 150–250 bpm
- P waves may be hidden, inverted, or appear after the QRS
- Distinction between AVNRT and AVRT often made via electrophysiologic studies
2. Ambulatory Monitoring
- Holter Monitor: Continuous 24–48 hour recording
- Event Recorder or Loop Recorder: For infrequent episodes
3. Echocardiography
- Assesses for structural heart disease or valve abnormalities
4. Electrophysiology (EP) Study
- Gold standard for mapping the reentrant circuit or ectopic focus
- Often precedes catheter ablation
Acute and Long-Term Management of SVT
Acute Termination of SVT
Non-Pharmacologic Interventions
- Vagal Maneuvers:
- Valsalva maneuver
- Carotid sinus massage (avoid in elderly or those with carotid disease)
- Modified Valsalva: Proven to be more effective in emergency settings
Pharmacologic Therapy
- Adenosine (First-line): Rapid IV push with saline flush; transient AV block helps terminate AVNRT/AVRT
- Beta-blockers or calcium channel blockers: For AV node-dependent arrhythmias
Electrical Cardioversion
- Synchronized shock for hemodynamically unstable patients
Long-Term Treatment and Prevention
Medication-Based Management
- Beta-blockers or nondihydropyridine calcium channel blockers for rate control
- Class IC (e.g., flecainide) or Class III (e.g., sotalol, amiodarone) agents for rhythm control
Catheter Ablation
- Curative in most AVNRT/AVRT cases
- Involves radiofrequency or cryoablation of abnormal conduction pathways
- High success rates (>95%) with low recurrence
Lifestyle Modifications
- Avoid stimulants (caffeine, alcohol, nicotine)
- Manage stress and anxiety
- Treat underlying conditions (thyroid disease, sleep apnea)
Prognosis and Long-Term Outlook
- Benign Course in Most: Especially with AVNRT or AVRT in structurally normal hearts
- Potential Complications:
- Tachycardia-induced cardiomyopathy
- Heart failure with frequent or prolonged episodes
- Sudden cardiac death is rare, except in pre-excited AF in WPW syndrome
Early diagnosis and treatment, particularly with curative catheter ablation, significantly improve quality of life and prevent progression or recurrence.
Special Considerations
Pediatric SVT
- Often presents as AVRT due to congenital pathways
- Responds well to adenosine or vagal maneuvers
- Ablation considered in older children or refractory cases
SVT During Pregnancy
- Vagal maneuvers and beta-blockers are first-line
- Ablation reserved for drug-refractory, symptomatic cases
- Adenosine is considered safe for acute termination
Advanced and Emerging Therapies
- 3D Mapping Systems: Increase precision during ablation
- Cryoballoon Ablation: Especially in atrial tachycardia
- Wearable ECG Monitors: Enhance early detection and remote diagnosis
- AI-Based Arrhythmia Detection: Facilitates rapid triage and follow-up
Supraventricular tachycardia represents a manageable yet impactful cardiac rhythm disorder. With advances in electrophysiology and noninvasive diagnostics, outcomes have greatly improved. A tailored approach combining acute management, preventive therapy, and, when appropriate, catheter ablation ensures both safety and symptom resolution for patients across age groups and clinical contexts.