Supraventricular arrhythmias refer to abnormal heart rhythms that originate above the ventricles, specifically in the atria or the atrioventricular (AV) node. These arrhythmias range from benign palpitations to life-altering rhythm disturbances that increase the risk of stroke, heart failure, and other complications. A thorough understanding of their classification, mechanisms, and therapeutic strategies is essential for optimal patient care.
Classification of Supraventricular Arrhythmias
Supraventricular arrhythmias are classified based on their site of origin and electrophysiologic characteristics. Major types include:
1. Atrial Fibrillation (AF)
- Pathophysiology: Chaotic atrial activity leading to ineffective atrial contraction
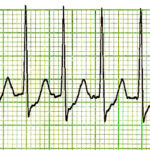
- ECG Findings: Irregularly irregular rhythm, absence of P waves
- Clinical Significance: Increased risk of thromboembolism and stroke
2. Atrial Flutter
- Pathophysiology: Reentrant circuit typically in the right atrium
- ECG Findings: Sawtooth flutter waves, especially in inferior leads
- Types: Typical (counterclockwise) and atypical (clockwise or left atrial origin)
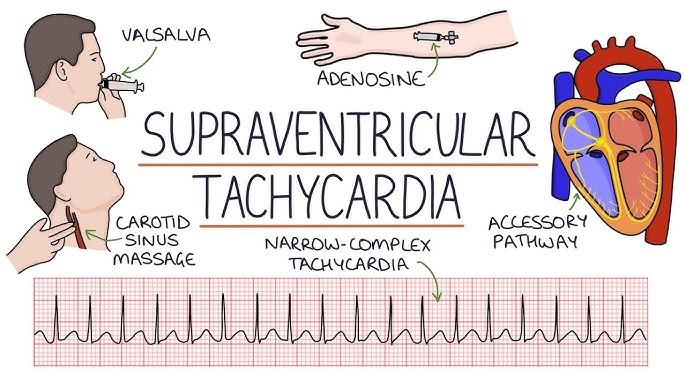
3. Paroxysmal Supraventricular Tachycardia (PSVT)
- Mechanism: Reentry involving the AV node or accessory pathways
- Subtypes:
- AV Nodal Reentrant Tachycardia (AVNRT)
- AV Reentrant Tachycardia (AVRT), e.g., Wolff-Parkinson-White syndrome
4. Multifocal Atrial Tachycardia (MAT)
- Features: Irregular rhythm with at least three different P-wave morphologies
- Often seen in: Chronic lung disease, electrolyte imbalance
5. Sinus Tachycardia and Inappropriate Sinus Tachycardia
- Description: Increased rate from the sinus node without reentry
- Causes: Physiologic or autonomic dysregulation
Common Symptoms of Supraventricular Arrhythmias
- Palpitations
- Dizziness or lightheadedness
- Syncope or presyncope
- Chest discomfort or pain
- Dyspnea
- Fatigue
- Anxiety (due to awareness of irregular heartbeats)
Risk Factors and Underlying Causes
- Hypertension and coronary artery disease
- Heart valve disorders
- Congenital heart abnormalities
- Thyroid dysfunction (especially hyperthyroidism)
- Sleep apnea
- Alcohol use (e.g., “holiday heart syndrome”)
- Stimulants: caffeine, nicotine, recreational drugs
Diagnostic Evaluation of Supraventricular Arrhythmias
1. Electrocardiography (ECG)
The cornerstone of arrhythmia diagnosis, providing rhythm characterization and identifying conduction anomalies.
2. Holter Monitoring or Event Recorders
Continuous or intermittent monitoring for paroxysmal or intermittent arrhythmias not captured on a standard ECG.
3. Echocardiography
Assesses structural abnormalities, chamber size, valvular integrity, and ejection fraction.
4. Electrophysiological (EP) Study
Used in complex cases for precise mapping and localization of arrhythmogenic foci.
5. Laboratory Investigations
- Thyroid function tests
- Electrolyte panel
- Renal function and BNP (if heart failure suspected)
Management Strategies for Supraventricular Arrhythmias
1. Acute Management
- Vagal Maneuvers: Carotid massage, Valsalva technique (for PSVT)
- Pharmacologic: Adenosine (PSVT), Beta-blockers, Calcium channel blockers
- Electrical Cardioversion: For unstable patients or refractory AF/flutter
2. Long-Term Rhythm Control
- Antiarrhythmic drugs: Amiodarone, flecainide, sotalol (depending on structural heart status)
- Catheter Ablation:
- First-line for AVNRT and AVRT
- Effective for atrial flutter and increasingly used for atrial fibrillation
3. Rate Control
- Appropriate for AF with persistent rhythm disturbance
- Agents include beta-blockers, diltiazem, or digoxin
4. Stroke Prevention
- CHA₂DS₂-VASc Score used to assess risk and guide anticoagulation decisions
- Anticoagulants: Warfarin, apixaban, rivaroxaban, dabigatran
5. Lifestyle and Risk Factor Modification
- Control of hypertension, diabetes, and sleep apnea
- Alcohol and stimulant avoidance
- Weight loss in obese patients
Prognosis and Complications
- Atrial Fibrillation: Increased risk of stroke, heart failure, dementia
- Atrial Flutter: Often progresses to AF if untreated
- PSVT: Generally benign but recurrent episodes can impair quality of life
- Inappropriate Sinus Tachycardia: Often difficult to treat; may require specialized care
Prompt diagnosis and appropriate treatment significantly improve prognosis and reduce the risk of complications.
Emerging Therapies and Innovations
- Pulmonary vein isolation for drug-refractory atrial fibrillation
- Left atrial appendage occlusion devices (e.g., Watchman) for patients contraindicated for anticoagulation
- Wearable ECG monitors and AI-powered arrhythmia detection tools
- Gene-based risk stratification in familial arrhythmia syndromes
Multidisciplinary Approach is Crucial
Effective management of supraventricular arrhythmias demands an individualized, evidence-based approach that incorporates clinical evaluation, rhythm monitoring, and advanced therapeutic modalities. Collaboration among cardiologists, electrophysiologists, and primary care providers ensures optimal patient outcomes and reduces the long-term burden of arrhythmic complications.