Schizophrenia, a severe mental health disorder characterized by distorted thinking, hallucinations, and delusions, is often accompanied by significant mood disturbances. One of the most concerning aspects of schizophrenia is the high prevalence of suicidal behavior among those affected. Suicidal thoughts and actions in schizophrenia pose a serious challenge for both patients and healthcare providers, as they can lead to significant loss of life and long-term emotional distress for families and loved ones. This article provides an in-depth exploration of suicidal behavior in schizophrenia, focusing on the risk factors, symptoms, and effective treatment strategies.
Schizophrenia and Suicidal Behavior: The Link
Schizophrenia is a chronic and debilitating condition that affects how an individual thinks, feels, and behaves. The disorder is often marked by episodes of psychosis, which may involve hallucinations, delusions, and disorganized speech and behavior. Individuals with schizophrenia may also experience substantial mood disturbances, including depression and anxiety.
Suicidal behavior in schizophrenia is of significant concern, with studies showing that up to 10% of individuals with schizophrenia will die by suicide. Understanding the underlying causes and risk factors of suicidal behavior in schizophrenia is essential to improving patient care and preventing self-harm.
The High Risk of Suicide in Schizophrenia
The risk of suicide is notably higher in individuals with schizophrenia compared to the general population. This heightened risk is multifaceted, stemming from a combination of factors such as the severity of symptoms, the impact of chronic illness, and social isolation. Suicidal behavior is most common in individuals during the early stages of the disorder, particularly before receiving adequate treatment.
Factors Contributing to Suicidal Behavior in Schizophrenia
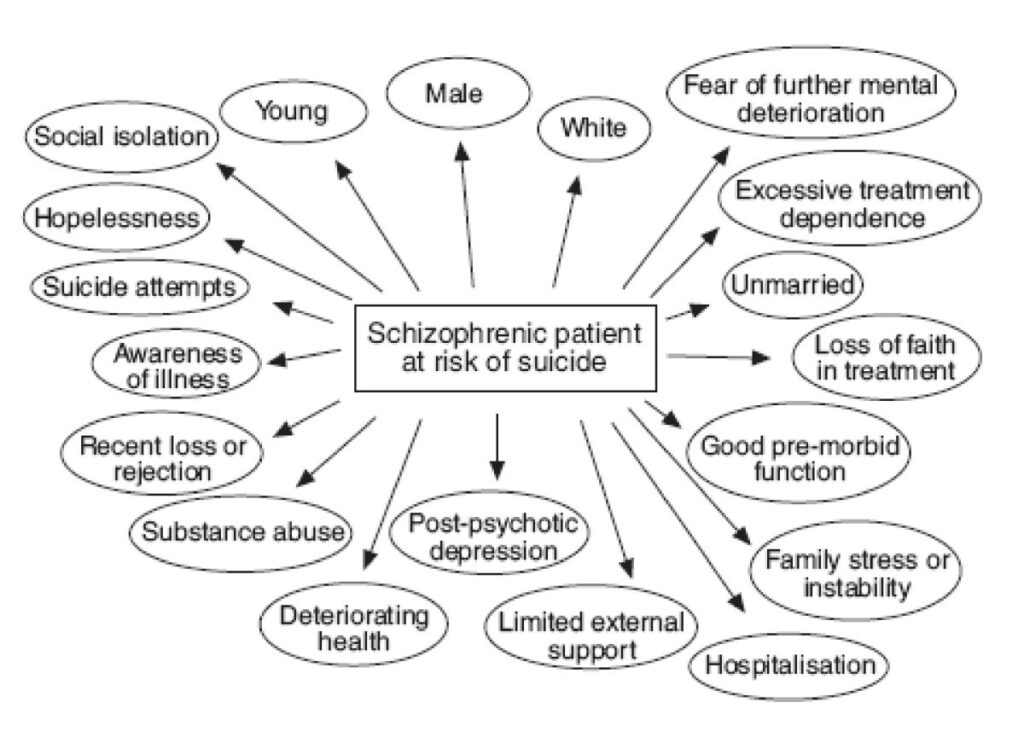
Suicidal behavior in schizophrenia is influenced by a combination of biological, psychological, and social factors. These factors can significantly alter the trajectory of the disorder and lead to severe outcomes if not addressed promptly.
Risk Factors for Suicidal Behavior in Schizophrenia
Several factors contribute to the elevated risk of suicidal behavior in individuals with schizophrenia. Understanding these risk factors is critical in identifying high-risk patients and intervening early.
1. Severity of Psychotic Symptoms
Psychotic symptoms, such as delusions and hallucinations, are central to the diagnosis of schizophrenia. These symptoms can distort an individual’s perception of reality, leading to intense emotional distress. For instance, individuals who experience persecutory delusions (e.g., believing that others are plotting against them) may become increasingly agitated, isolated, and fearful, which may heighten suicidal thoughts.
2. Depression and Comorbid Mood Disorders
Depression is one of the most common mood disturbances observed in individuals with schizophrenia. The depressive episodes in schizophrenia often coincide with feelings of hopelessness, worthlessness, and despair—key risk factors for suicidal behavior. Additionally, comorbid mood disorders, such as bipolar disorder, are common in schizophrenia, further complicating the situation.
3. Previous Suicide Attempts
A history of prior suicide attempts is one of the most significant risk factors for future suicidal behavior. Research indicates that individuals with schizophrenia who have previously attempted suicide are at much higher risk of repeating such behavior. Therefore, it is crucial to monitor patients with a history of suicidal behavior closely.
4. Substance Abuse
Substance abuse, particularly alcohol and drugs, is frequently observed in individuals with schizophrenia. The use of substances can exacerbate psychotic symptoms, impair judgment, and increase impulsivity, which can all lead to a higher risk of suicide. Substance abuse may also prevent patients from adhering to their treatment plans, which exacerbates the progression of the disorder.
5. Social Isolation and Lack of Support
Schizophrenia often leads to significant social isolation due to the severity of symptoms and difficulty in maintaining relationships. Social withdrawal can cause feelings of loneliness and alienation, which are risk factors for suicidal thoughts and behavior. Without a strong support system, individuals may feel overwhelmed by their condition and resort to self-harm.
Symptoms of Suicidal Behavior in Schizophrenia
Recognizing the signs of suicidal behavior is crucial in preventing tragic outcomes. The symptoms of suicidal behavior in individuals with schizophrenia can be subtle but should be taken seriously. Early intervention can help reduce the risk and improve the overall prognosis.
Common Symptoms of Suicidal Ideation
- Verbalizing Suicidal Thoughts: Expressions such as “I don’t want to live anymore” or “The world would be better off without me” are red flags for potential suicidal behavior.
- Behavioral Changes: Sudden withdrawal from activities, social isolation, and neglect of personal hygiene can indicate a decline in mental health and an increased risk of suicide.
- Mood Swings and Irritability: Extreme mood fluctuations, particularly irritability or sudden sadness, may be indicative of internal emotional turmoil.
- Increased Substance Use: A spike in alcohol or drug consumption may signal an attempt to self-medicate or escape distressing symptoms.
- Giving Away Possessions: A person who is preparing for death may begin to give away their belongings or make final arrangements, which is a strong indication of suicidal intent.
Treatment Strategies for Suicidal Behavior in Schizophrenia
Effectively managing suicidal behavior in schizophrenia requires a comprehensive and individualized approach. A combination of pharmacological treatments, psychotherapy, and community support is essential to addressing the complex needs of patients at risk.
1. Antipsychotic Medications
Antipsychotic medications are the cornerstone of schizophrenia treatment. These medications help manage psychotic symptoms, such as delusions and hallucinations, which can otherwise contribute to suicidal thoughts. Antipsychotics are available in both first-generation (typical) and second-generation (atypical) forms. Second-generation antipsychotics are preferred due to their superior side effect profile and greater efficacy in managing mood symptoms.
2. Mood Stabilizers and Antidepressants
When depression is a significant component of the individual’s condition, the addition of mood stabilizers and antidepressants is essential. Lithium, anticonvulsants, and antidepressants are commonly prescribed to address mood instability and depressive episodes, both of which can trigger suicidal thoughts.
3. Psychotherapy
Psychotherapy, particularly cognitive-behavioral therapy (CBT), plays a pivotal role in managing suicidal behavior in schizophrenia. CBT helps patients identify and challenge negative thought patterns and develop healthier coping mechanisms. Other therapeutic approaches, such as dialectical behavior therapy (DBT), may be used for individuals with emotional regulation issues and impulsive behaviors.
4. Crisis Intervention and Inpatient Care
In cases where patients are at immediate risk of self-harm, crisis intervention strategies are vital. Inpatient care and 24/7 monitoring may be required to ensure the patient’s safety and provide intensive psychiatric support. Hospitalization provides a controlled environment where healthcare professionals can manage acute symptoms and develop a tailored treatment plan.
5. Long-Term Monitoring and Support
Long-term care involves regular follow-ups, continuous medication management, and psychosocial support. Ongoing therapy, coupled with involvement in support groups or community resources, plays a critical role in preventing relapse and sustaining recovery.
Suicidal behavior in schizophrenia remains a significant challenge in mental health care. With the right combination of pharmacological treatment, psychotherapy, and social support, individuals with schizophrenia can be effectively managed, and the risk of suicide can be minimized. Identifying risk factors early, implementing comprehensive care plans, and ensuring continuous support are essential steps in improving the lives of those affected by this devastating condition.