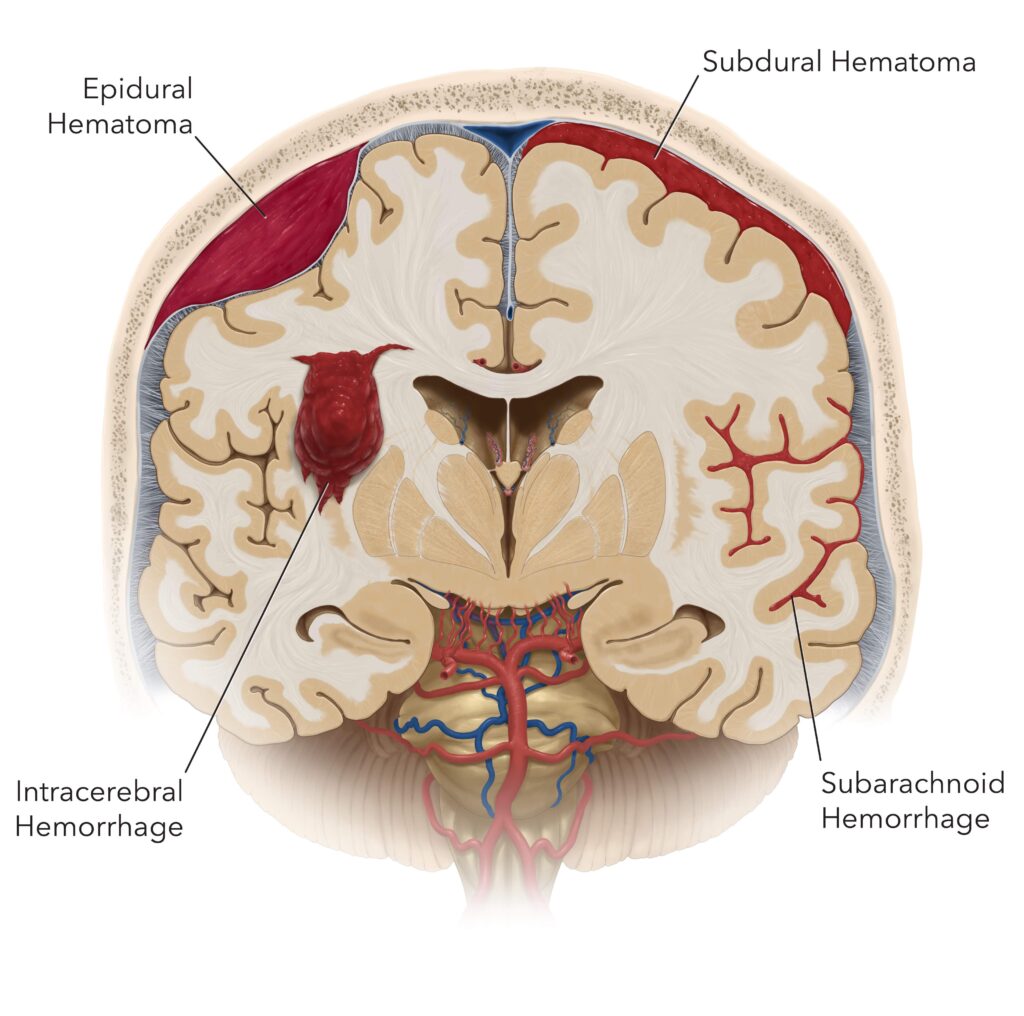
Subarachnoid intracranial hemorrhage (SAH) is a rare but serious condition in which bleeding occurs in the subarachnoid space, the area between the brain and the thin tissues covering it. This type of hemorrhage can lead to severe complications, including brain injury, coma, or even death, making early detection and treatment crucial. Understanding the causes, symptoms, diagnosis, and treatment options for subarachnoid hemorrhage can significantly improve outcomes and help in the management of this life-threatening condition.
What Causes Subarachnoid Hemorrhage?
Subarachnoid hemorrhage can result from various factors, most commonly trauma or rupture of an aneurysm. Understanding these causes is vital for prevention and prompt intervention.
1. Aneurysm Rupture
The most common cause of spontaneous subarachnoid hemorrhage is the rupture of an aneurysm, a weakened area in the wall of a blood vessel in the brain. When an aneurysm bursts, it releases blood into the subarachnoid space, which can lead to a range of symptoms, including a sudden, severe headache. These aneurysms often occur at points where blood vessels branch, making them vulnerable to rupture.
- Congenital Aneurysms: Some individuals may be born with weakened blood vessel walls that predispose them to aneurysms.
- Acquired Aneurysms: Factors such as high blood pressure, smoking, or infections can cause aneurysms to form over time.
2. Traumatic Injury
Head trauma, such as a blow to the head from an accident or fall, can lead to subarachnoid hemorrhage. In these cases, the bleeding may result from direct damage to the blood vessels in the brain.
- Motor Vehicle Accidents: A common cause of head trauma leading to hemorrhage.
- Falls: Falls, particularly in elderly individuals, can result in significant brain injury.
3. Arteriovenous Malformation (AVM)
Arteriovenous malformations, which are abnormal tangles of blood vessels, can also lead to subarachnoid hemorrhage. These malformations often present with symptoms as the abnormal vessels weaken and rupture.
4. Hypertension
Chronic high blood pressure is a significant risk factor for the rupture of blood vessels in the brain, particularly in individuals with pre-existing vascular issues. Over time, the blood vessel walls may become damaged and more susceptible to hemorrhage.
5. Coagulopathy and Blood Thinning Medications
Conditions that affect blood clotting, such as anticoagulant use or bleeding disorders, can increase the risk of subarachnoid hemorrhage. Medications like warfarin, while useful for preventing strokes, may also increase the likelihood of hemorrhaging when blood vessels rupture.
6. Infections and Inflammatory Conditions
In rare cases, infections in the brain, such as meningitis or encephalitis, can lead to inflammation and weakening of blood vessels, contributing to the development of subarachnoid hemorrhage.
Symptoms of Subarachnoid Hemorrhage
The hallmark of subarachnoid hemorrhage is a sudden, intense headache, often described as the worst headache a person has ever experienced. However, other symptoms may accompany the condition, depending on the severity and location of the bleeding.
1. Severe Sudden Headache
The “thunderclap” headache is a defining characteristic of subarachnoid hemorrhage. This excruciating headache typically comes on suddenly and reaches its peak intensity within seconds to minutes. It may be localized to one part of the head or feel like a generalized headache.
2. Neck Stiffness and Pain
Due to the irritation of the meninges (the protective membranes surrounding the brain), individuals may experience severe neck pain and stiffness. This symptom is often accompanied by nausea and vomiting.
3. Loss of Consciousness
Depending on the severity of the hemorrhage, individuals may lose consciousness either briefly or for longer periods. A person may become disoriented, drowsy, or unresponsive, and in severe cases, may fall into a coma.
4. Seizures
Seizures can occur in some individuals following a subarachnoid hemorrhage due to abnormal electrical activity in the brain. These may manifest as involuntary muscle jerking or loss of motor control.
5. Vision Problems
Blurred vision or double vision can result from the pressure exerted on certain parts of the brain during the hemorrhage. Photophobia (sensitivity to light) is also a common symptom.
6. Speech and Cognitive Issues
Difficulty speaking, confusion, or memory loss may occur if the hemorrhage affects regions of the brain involved in cognition and speech. In some cases, individuals may experience paralysis or weakness in one part of the body (hemiparesis).
Diagnosis of Subarachnoid Hemorrhage
Accurate and timely diagnosis of subarachnoid hemorrhage is crucial for initiating treatment. A combination of imaging studies and physical exams is typically used to confirm the presence of bleeding in the brain.
1. CT Scan (Computed Tomography)
A CT scan is the first-line imaging test used to diagnose subarachnoid hemorrhage. This non-invasive procedure can rapidly detect the presence of blood in the subarachnoid space. The scan is highly effective in identifying hemorrhages within the first 24-48 hours after onset.
2. MRI (Magnetic Resonance Imaging)
MRI scans may be used to identify smaller hemorrhages or brain injuries that a CT scan might miss. This method provides a more detailed view of the brain’s soft tissues and is especially useful in detecting aneurysms or vascular malformations.
3. Cerebral Angiography
In cases where the source of bleeding is unclear, cerebral angiography is used to visualize blood vessels in the brain. This test involves injecting a contrast dye into the blood vessels and using X-ray technology to detect any abnormalities such as aneurysms or arteriovenous malformations.
4. Lumbar Puncture (Spinal Tap)
In some cases, a lumbar puncture may be performed if the CT scan is inconclusive. The presence of blood or xanthochromia (yellow-tinged cerebrospinal fluid) can indicate a subarachnoid hemorrhage.
Treatment of Subarachnoid Hemorrhage
The treatment of subarachnoid hemorrhage aims to control bleeding, prevent complications, and restore normal brain function. The specific approach depends on the underlying cause, severity, and individual patient factors.
1. Emergency Care and Stabilization
Initial management focuses on stabilizing the patient’s condition. This includes ensuring adequate oxygenation, controlling blood pressure, and preventing further brain injury. In some cases, medications may be used to prevent vasospasm (narrowing of blood vessels) and seizures.
2. Surgical Intervention
Surgery is often necessary to address the cause of the hemorrhage, especially if it results from an aneurysm or arteriovenous malformation. Surgical options include:
- Aneurysm Clipping: A procedure where the aneurysm is isolated and sealed off to prevent further bleeding.
- Endovascular Coiling: A minimally invasive technique where a coil is inserted into the aneurysm to promote clotting and prevent rupture.
- Craniotomy: In some cases, a craniotomy may be required to access and repair damaged blood vessels.
3. Medications
Medications to control blood pressure, prevent seizures, and reduce the risk of complications such as brain swelling are often prescribed. Calcium channel blockers like nimodipine are used to prevent vasospasm, which can reduce blood flow to the brain and cause ischemic injury.
4. Rehabilitation
After initial treatment, individuals may require physical therapy, speech therapy, or cognitive therapy to regain lost functions. Rehabilitation helps patients recover mobility, speech, and cognitive abilities that may have been impaired by the hemorrhage.
Prognosis of Subarachnoid Hemorrhage
The prognosis of subarachnoid hemorrhage depends on several factors, including the severity of the hemorrhage, the speed of treatment, and the underlying cause. Prompt intervention can improve outcomes significantly, but in some cases, the damage may be irreversible.
- Early Treatment: Patients who receive prompt treatment have a better chance of survival and recovery.
- Complications: Vasospasm, rebleeding, and hydrocephalus (accumulation of cerebrospinal fluid) can complicate recovery and affect long-term prognosis.
- Long-Term Recovery: Some individuals may experience long-term neurological deficits, including cognitive impairments or motor weaknesses.
Prevention of Subarachnoid Hemorrhage
While not all cases of subarachnoid hemorrhage can be prevented, certain strategies can reduce the risk, particularly for individuals with known risk factors.
1. Managing Blood Pressure
Controlling high blood pressure is essential in preventing the rupture of blood vessels in the brain. Regular monitoring and medications may be necessary for individuals with hypertension.
2. Avoiding Smoking and Excessive Alcohol Consumption
Smoking and excessive alcohol consumption increase the risk of aneurysm formation and rupture. Quitting smoking and moderating alcohol intake are key steps in reducing the risk of subarachnoid hemorrhage.
For individuals with a family history of brain aneurysms or other risk factors, regular screening with MRI or CT angiography may help detect aneurysms before they rupture.
Subarachnoid intracranial hemorrhage is a severe and potentially life-threatening condition that requires immediate medical attention. Early diagnosis, prompt treatment, and preventive measures can significantly improve outcomes for patients. By understanding the causes, symptoms, diagnosis, treatment options, and preventive strategies, healthcare professionals and individuals can better manage the risks associated with this condition.