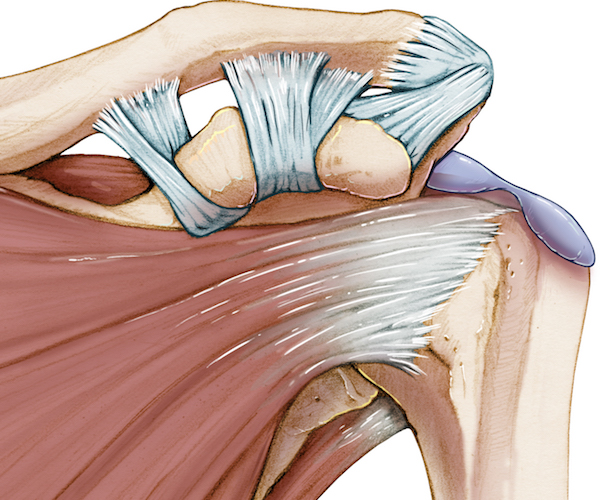
Subacute bursitis refers to the inflammation of a bursa that persists beyond the acute phase, but without the severity typically associated with chronic bursitis. The bursa is a small, fluid-filled sac located around joints that serves to cushion and reduce friction between bones, tendons, and muscles. When these sacs become irritated or inflamed, the condition is referred to as bursitis. Subacute bursitis falls in the middle of the spectrum of this condition, where symptoms are present but not as severe or long-lasting as in chronic bursitis.
This condition can affect various joints, including the shoulders, elbows, hips, knees, and more, causing discomfort, limited mobility, and swelling. Early diagnosis and treatment are essential to manage symptoms effectively and prevent progression to chronic bursitis.
Understanding the Causes of Subacute Bursitis
Subacute bursitis is often the result of an injury or repetitive motion, though it can also develop due to infection or underlying medical conditions. The following are the most common causes of subacute bursitis:
1. Overuse or Repetitive Stress
Overuse is a primary contributor to bursitis, especially when certain joints are subjected to repetitive motion or excessive strain. Activities such as frequent kneeling, throwing, or lifting heavy objects can irritate the bursa and trigger inflammation.
- Occupational Risks: Jobs or activities that involve repetitive arm, elbow, or knee movements can lead to increased wear and tear on the bursa.
- Sports-related Injuries: Athletes involved in high-impact sports or repetitive motions (e.g., tennis, baseball) are at higher risk.
2. Trauma or Injury
A direct blow or injury to the area around a bursa can lead to subacute bursitis. Even minor trauma, such as a fall or bump, can trigger inflammation that takes time to resolve.
3. Infection
Though less common, bursitis can become infected, leading to a condition known as septic bursitis. Bacterial infections, such as those caused by Staphylococcus aureus, can lead to swelling, pain, and redness in the affected area.
4. Underlying Health Conditions
Certain medical conditions can make individuals more susceptible to bursitis. These include:
- Rheumatoid arthritis: Inflammatory conditions like rheumatoid arthritis can cause bursa inflammation.
- Gout: The accumulation of uric acid crystals in the joints can trigger gouty bursitis.
- Diabetes: People with diabetes may experience changes in circulation and immune response that increase the risk of bursitis.
5. Age-Related Factors
As people age, the tissues around the joints, including the bursa, may become less elastic and more prone to injury. This makes older adults more susceptible to conditions like subacute bursitis.
Symptoms of Subacute Bursitis
The symptoms of subacute bursitis can vary in intensity and may not be as pronounced as in the acute phase, but they can still affect daily activities and mobility. Common symptoms include:
1. Pain and Tenderness
Pain is a hallmark of bursitis, and in subacute cases, it may persist after the initial injury or inflammation. The pain is typically dull or aching, and it may increase with certain movements or pressure on the affected joint.
- Location-Specific Pain: The pain is localized to the area of the affected bursa, such as the elbow (olecranon bursitis) or the knee (prepatellar bursitis).
- Pain with Movement: Engaging in activities that require bending or stretching the affected joint can intensify the discomfort.
2. Swelling and Inflammation
While the swelling in subacute bursitis may not be as severe as in acute cases, there is still noticeable swelling around the affected bursa. The area may feel warm to the touch, and the swelling may increase with activity.
3. Limited Range of Motion
Increased swelling and pain can limit the range of motion of the affected joint. For example, individuals with shoulder bursitis may find it difficult to lift their arm above the head or engage in overhead activities.
4. Redness and Warmth
If the bursitis is related to an infection or irritation, the affected area may appear red and feel warm. This symptom is particularly noticeable in septic bursitis, where the infection causes inflammation.
Diagnosis of Subacute Bursitis
Diagnosing subacute bursitis typically involves a combination of physical examination, imaging studies, and sometimes laboratory tests. Early detection is key to effective management, preventing further inflammation, and addressing any underlying issues.
1. Physical Examination
During the physical exam, a healthcare provider will assess the affected joint for signs of swelling, tenderness, and limited movement. They may also apply gentle pressure around the bursa to check for pain or discomfort.
2. Imaging Tests
In many cases, imaging tests are used to confirm the diagnosis and rule out other conditions that may cause similar symptoms:
- X-rays: While X-rays do not show soft tissue problems directly, they may help rule out other joint or bone issues.
- Ultrasound: This non-invasive imaging technique can be used to assess fluid accumulation and inflammation in the bursa.
- MRI: In more complex cases, MRI scans may be used to visualize deeper tissue and assess the severity of inflammation.
3. Laboratory Tests
If an infection is suspected, a healthcare provider may recommend a culture test to determine if bacteria are present in the bursa. Blood tests may also be used to check for elevated white blood cell counts, which indicate inflammation or infection.
Treatment of Subacute Bursitis
The treatment of subacute bursitis focuses on reducing inflammation, relieving pain, and preventing further joint damage. Treatment can be conservative or more invasive, depending on the severity of the condition.
1. Rest and Activity Modification
The first step in treating subacute bursitis is to reduce the strain on the affected joint. This may involve:
- Resting the Joint: Avoid activities that aggravate the symptoms, such as repetitive movements or heavy lifting.
- Applying Ice: Ice packs can help reduce swelling and numb the pain in the affected area.
2. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs, such as ibuprofen or naproxen, are commonly used to reduce inflammation and alleviate pain. These medications are effective for managing mild to moderate symptoms of bursitis.
3. Corticosteroid Injections
If pain and inflammation persist despite rest and NSAIDs, corticosteroid injections may be administered directly into the bursa. These injections provide more targeted relief and help reduce inflammation in the affected area.
4. Physical Therapy
Physical therapy is often recommended to restore movement and strength in the joint. Exercises that improve flexibility and strengthen the surrounding muscles can prevent future episodes of bursitis.
5. Surgical Treatment
In rare cases where conservative treatments fail to provide relief, surgery may be necessary. This is typically reserved for chronic bursitis or when there is significant damage to the bursa.
Prevention of Subacute Bursitis
Preventing subacute bursitis involves managing risk factors and protecting the joints from overuse and trauma. Key prevention strategies include:
1. Warm-up Before Physical Activity
Always engage in proper warm-up exercises before participating in sports or physical activities. Stretching and mobility exercises can help reduce the risk of joint strain and injury.
2. Avoid Repetitive Stress
If your job or activity involves repetitive movements, take regular breaks to rest your joints. Modify your technique or use assistive devices to reduce the strain on your joints.
3. Strengthen Muscles Around Joints
Maintaining strong muscles around the joints provides better support and helps protect the bursa from stress. Regular strength training exercises are essential for joint health.
4. Use Proper Equipment
If you engage in sports or activities that put stress on your joints, using proper equipment, such as knee pads or elbow supports, can help reduce the risk of bursitis.
Subacute bursitis is a manageable condition that can cause significant discomfort and impair daily activities. By understanding its causes, recognizing the symptoms, and seeking timely treatment, individuals can effectively manage the condition and prevent its progression to chronic bursitis. Early intervention, along with proper rest, medication, and physical therapy, is crucial in ensuring a full recovery and reducing the risk of future flare-ups.